Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 2 items
A 25-year-old man comes to the emergency department because of headache, palpitations, sweating, and irritability. He came directly from the health club, which he joined a few weeks ago. He states that after every exercise session during evening, before dinner, he develops similar symptoms and he gets symptomatic relief by consuming granola bars. He was diagnosed with type 1 diabetes mellitus eight years ago. He takes a combination of NPH and regular insulin before breakfast and supper. He states that he is very compliant with his insulin and meals. He does not have any other symptoms or chronic complications of diabetes. His blood pressure is 110/80 mmHg, pulse is 100/min, temperature is 36.7C (98F) and respirations are 14/min. He is slightly diaphoretic but completely alert and awake. His neurological examination is nonfocal. The rest of the examination is unremarkable.
Item 1 of 2
Hypoglycemia is defined as a plasma glucose level of:
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 2
Which of the following is the most appropriate step to prevent further hypoglycemic episodes in this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
A 46-year-old woman comes to the office due to frequent episodes of headache, nausea, sweating, and a feeling as if she is going to pass out. The patient has had 3 such episodes in the past 2 weeks, with symptoms occurring when she skips a meal. During the most recent episode, finger-stick glucose was 50 mg/dL. She was diagnosed with type 2 diabetes mellitus 3 years ago and initially treated with metformin monotherapy; glipizide was added 3 months ago due to inadequate glycemic control. The patient has no other medical conditions. Vital signs are within normal limits and physical examination shows no abnormalities. Hemoglobin A1c is 6.9%. The medication most likely responsible for this patient’s current symptoms works by targeting which of the following?
CorrectIncorrect -
Question 4 of 40
4. Question
A 68-year-old woman comes to the emergency department due to a month-long history of increasing palpitations. She has had no associated chest pain or shortness of breath but has experienced unusual fatigability. The patient has also noted a 4-kg (8.8-lb) weight loss on her home scale and has been waking with increasing frequency at night to urinate. She was diagnosed with osteopenia on bone densitometry at age 65; she increased her intake of “milk, yogurt, cheese, and other foods with lots of calcium” and started a vitamin D supplement, but repeat DXA 2 months ago revealed a significant interval decline in bone density. The patient’s medical history is otherwise unremarkable, and she does not use tobacco, alcohol, or illicit drugs. Her mother died of breast cancer at age 62 and her father died in a motor vehicle collision at age 40. Temperature is 36.7 C (98 F), blood pressure is 151/68 mm Hg, pulse is 122/min, and respirations are 16/min. The thyroid gland is diffusely enlarged and nontender. Lid lag is noted on eye examination. The lungs are clear to auscultation. The heart has an irregularly irregular tachycardia with a variable intensity of S1. Laboratory results are as follows:
Serum chemistries
Sodium
142 mEq/L
Potassium
3.6 mEq/L
Bicarbonate
23 mEq/L
Urea nitrogen
15 mg/dL
Creatinine
0.8 mg/dL
Glucose
122 mg/dL
Calcium
10.3 mg/dL
Complete blood count
Hemoglobin
13.1 g/dL
Leukocytes
9,800/mm3
Platelets
330,000/mm3
TSH
<0.01 μU/mL
Free T4
4.7 ng/dL (0.9-2.4 ng/dL)
Which of the following should be addressed next in treatment of this patient’s condition?
CorrectIncorrect -
Question 5 of 40
5. Question
A 63-year-old man comes to the office for follow-up on abnormal test results. He was found to have a blood glucose level of 255 mg/dL during a recent outpatient visit. The patient previously had normal blood glucose levels, except during a hospital admission for abdominal pain 9 months ago, when he briefly required insulin for hyperglycemia. He now has dry mouth and frequent urination and has lost 10.4 kg (22.9 lb) in the last 6 months. Medical history includes chronic pancreatitis from alcohol use disorder, hypertension, and chronic kidney disease. He quit drinking alcohol a year ago. Both of his parents had type 2 diabetes mellitus. Blood pressure is 132/80 mm Hg and pulse is 76/min. BMI is 24 kg/m2. Physical examination shows mild bilateral pedal edema. Repeat blood glucose level is 250 mg/dL, hemoglobin A1c is 8.5%, and estimated glomerular filtration rate is 28 mL/min/1.73 m2. Which of the following medications is most appropriate for treatment of diabetes mellitus in this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
A 40-year-old man is brought to the emergency department for sudden onset of headaches, diaphoresis, and loss of consciousness. His wife states that he was previously in his usual state of health. His past medical history is unremarkable. He works as a physician assistant and does not smoke or drink alcohol. On physical examination, the patient is diaphoretic and comatose. His fingerstick blood glucose level is 45 mg/dL. The patient is given 50% dextrose intravenously and then regains consciousness. He says that he is currently dealing with a great deal of work- and relationship-related stress.
Laboratory test results on the blood sample drawn prior to dextrose administration are as follows:
Blood glucose 42 mg/dL Serum insulin Elevated C-peptide level Elevated Proinsulin Elevated Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
A 67-year-old man comes for follow-up of coronary artery disease. He is currently feeling well. Three months ago, he was hospitalized for chest pain; coronary angiography revealed 85% narrowing in the mid right coronary artery, and a drug-eluting stent was placed. In addition, TSH was noted to be low. The patient now walks 2-3 miles a day without angina, dyspnea, or lower extremity claudication. He states, “I am very happy that I lost 5 lb since my hospitalization. I also gave up smoking and drinking. I feel like I got my life back.” Current medications include aspirin, clopidogrel, metoprolol, lisinopril, and atorvastatin. The patient’s father died from a heart attack at age 56, and his mother has osteoporosis and hypertension. Blood pressure is 134/76 mm Hg and pulse is 65/min. BMI is 28 kg/m2. Physical examination, including examination of the thyroid gland, is normal. Repeat thyroid function results are as follows:
During hospitalization
Current
TSH
0.14 µU/mL
0.08 µU/mL
Free T4
1.8 ng/dL
1.74 ng/dL (normal: 0.9-2.4)
Total T3
88 ng/dL
133 ng/dL
Radioactive iodine uptake is increased, with a homogeneous distribution on thyroid scan. Which of the following is the most appropriate management for this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
A 35-year-old woman is being evaluated for uncontrolled hypertension. She was recently diagnosed with diabetes mellitus. Medical history is significant for mood swings. Temperature is 36.7 C (98 F), blood pressure is 150/100 mm Hg, pulse is 88/min, and respirations are 14/min. Lungs are clear on auscultation bilaterally, and the heart rhythm is regular. Abdominal auscultation fails to reveal any bruit. All peripheral pulsations are full. Laboratory results are as follows:
Sodium 140 mEq/L Potassium 3.4 mEq/L Bicarbonate 30 mEq/L Blood urea nitrogen 20 mg/dL Creatinine 0.8 mg/dL Calcium 9.5 mg/dL Blood glucose 198 mg/dL Chest x-ray is suggestive of dorsal vertebral osteopenia. Which of the following is the most appropriate investigation?
CorrectIncorrect -
Question 9 of 40
9. Question
The following vignette applies to the next 2 items.
A 54-year-old woman comes to the emergency department with palpitations. She has experienced paroxysmal atrial fibrillation for the past 6 months. She has had extensive investigations for an underlying cause, including echocardiography and thyroid function testing, which were normal. The patient was started on amiodarone 6 weeks ago by her cardiologist and did well in the interim. She has had no change in her weight or intolerance to hot or cold temperatures. Her other medications include atenolol and low-dose aspirin. On physical examination, the patient appears comfortable. Her blood pressure is 132/82 mm Hg and heart rate is 112/min and irregular. Laboratory studies show a normal complete blood count and basic metabolic panel. ECG shows atrial fibrillation with rapid ventricular response. Thyroid function markers are as follows:
TSH 4.5 mU/L (normal 0.35-5.0 mU/L) Total T4 15.6 μg/dL (normal 4-11 μg/dL) Total T3 75 ng/dL (normal 80-180 ng/dL) Item 1 of 2
What is the most likely explanation for this patient’s thyroid function tests?
CorrectIncorrect -
Question 10 of 40
10. Question
Item 2 of 2
What is the best management for this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 54-year-old woman is brought to the emergency department due to disorientation. She was recently on vacation and received treatment with high-dose oral prednisone for severe poison ivy dermatitis. In the emergency department, her temperature is 37 C (98.6 F), blood pressure is 138/80 mm Hg, pulse is 102/min, and respirations are 22/min. The mucous membranes are dry. Laboratory results show random blood glucose of 1020 mg/dL with a normal anion gap. Her hemoglobin A1c is 7.6%. The patient is started on intravenous fluids and an intravenous insulin infusion. After a day on intravenous insulin, her mental status is normal and she is transitioned to subcutaneous regular human insulin based on a sliding scale. Her finger stick blood glucose readings are 200-250 mg/dL. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 12 of 40
12. Question
A 45-year-old man comes to the clinic for follow-up of hypertension. The patient has been taking lisinopril since the condition was diagnosed 6 months ago. He has a 10-pack-year history; he quit smoking 5 years ago. Medical history includes laparoscopic cholecystectomy 5 years ago after an episode of acute cholecystitis. The patient does not consume alcohol. His father had a heart attack at age 62, and his mother died of a stroke at age 67. Blood pressure is 130/80 mm Hg and pulse is 67/min. BMI is 30 kg/m2. Physical examination is unremarkable. Fasting laboratory results are as follows:
Total cholesterol
250 mg/dL
Triglycerides
340 mg/dL
HDL
35 mg/dL
LDL
147 mg/dL
Glucose
98 mg/dL
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
A 65-year-old female is admitted to the intensive care unit for chest pain where she is diagnosed with a non-ST elevation myocardial infarction. She has a history of hypertension, type 2 diabetes mellitus, hyperlipidemia, and osteoporosis. Over the last two months, she has been getting occasional chest pain on exertion. She also complains of some recent fatigue and mild constipation. Cardiac catheterization is performed and shows severe triple-vessel coronary artery disease. A coronary artery bypass graft procedure (CABG) is planned. Her laboratory values include the following:
TSH
20 mU/L
Total T4
3.5 micro g/dL
Morning cortisol
20 micro g/dL
HbA1c
7.5%
Which of the following is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 19-year-old man comes to the office for a new patient visit. Three months ago, he was seen at an urgent care clinic due to fatigue, excessive urination, and unexpected weight loss. Laboratory evaluation at that time showed a serum glucose level of 384 mg/dL, normal anion gap, and hemoglobin A1c of 10.4%. Regular insulin was prescribed, which the patient takes before meals, and insulin glargine, which he takes at night. The patient checks his blood sugar 3 times daily; home glucose levels usually range from 100 to 300 mg/dL but have been as low as 65 mg/dL. He consumes a diabetic diet and tracks carbohydrate counts appropriately. He does not exercise. BMI is 24 kg/m2. Physical examination, including monofilament testing of the feet, is normal. Laboratory results are as follows:
Blood urea nitrogen
14 mg/dL
Serum creatinine
0.8 mg/dL
Fasting serum glucose
156 mg/dL
Hemoglobin A1c
9.2%
Urinalysis
Protein
negative
Glucose
negative
Ketones
negative
Which of the following is the best next step to promote optimal glycemic control in this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 75-year-old woman comes to the office with a 2-week history of palpitations, fatigue, heat intolerance, sweating, and weight loss. She was diagnosed with coronary artery disease 4 weeks ago after having chest pain. Coronary angiography revealed a high-grade stenosis in the right coronary artery; the patient was treated with angioplasty and stent placement and was discharged with prescriptions for aspirin, clopidogrel, atorvastatin, and metoprolol. She also has hypertension and type 2 diabetes mellitus, for which she takes hydrochlorothiazide, lisinopril, and metformin. The patient has a 20-pack-year smoking history but quit 10 years ago; she does not use alcohol or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 140/76 mm Hg, pulse is 120/min, and respirations are 18/min. Oxygen saturation by pulse oximetry is 96% on room air. On examination, the thyroid is slightly enlarged, firm, irregular, and nontender. There are no carotid bruits or jugular venous distension. The heart has a regular tachycardia with no murmurs or gallops. Bedside glucose is 130 mg/dL. ECG shows sinus tachycardia with no other significant abnormalities. The dose of the patient’s beta blocker is increased, and she is sent for laboratory studies. Complete blood count, electrolytes, and hepatic transaminases are normal. Total T3 and free T4 are elevated, and TSH is undetectable. Thyrotropin receptor antibody assay is negative. Thyroid ultrasound reveals a multinodular goiter with increased vascularity. On follow-up 2 days later, the patient reports only partial relief of symptoms. Blood pressure is 135/80 mm Hg and pulse is 105/min. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 24-year-old woman comes to the office due to localized swelling in the front of her neck. She has had no associated pain, difficulty swallowing, or voice changes. The patient is otherwise healthy and takes no medications; she has no history of radiation exposure or family history of thyroid disease. Physical examination shows firm swelling in the right side of the thyroid gland. Serum TSH and free thyroxine levels are normal. Thyroid ultrasonography reveals a solid nodule measuring 2.6 × 1.7 × 1.3 cm in the right lobe; the left lobe is normal in size and echotexture.
Item 1 of 2
Which of the following is the best next step in management of this patient?CorrectIncorrect -
Question 17 of 40
17. Question
Item 2 of 2
Fine-needle aspiration biopsy of the nodule shows nests of polygonal cells with extracellular, Congo red–positive amyloid deposits, findings consistent with medullary thyroid cancer. Serum calcitonin is 300 pg/mL (normal: 0-10). Genetic studies show a mutation in the RET protooncogene. Which of the following is the best next step in management of this patient?CorrectIncorrect -
Question 18 of 40
18. Question
A 62-year-old man comes to the office for follow-up for type 2 diabetes mellitus diagnosed 12 years ago. For the past year, his glycemic control has been suboptimal despite treatment with multiple noninsulin antihyperglycemic agents. The patient takes his prescribed medications consistently and follows recommended lifestyle changes. Examination of the feet is notable for a bilateral decrease in sensation on monofilament testing. The remainder of the physical examination is unremarkable. Hemoglobin A1c is 8.4% and serum creatinine is 1.4 mg/dL. The patient is counseled on the addition of insulin glargine as basal insulin. Which of the following is an advantage of using this therapy over NPH twice a day for this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
The following vignette applies to the next 2 items.
A 26-year-old woman comes to the office due to fever, sweating, heat intolerance, and shortness of breath. Her symptoms began a week ago and have become progressively worse. The patient has also had severe pain in the anterior neck, which radiates to the angle of the jaw and ears and is worse when she turns her head. She adds that she has “been under a lot of stress lately since I was laid off from my job. I have been babysitting to make some extra money, but I think one of the kids gave me ‘the flu.’ I had a runny nose, cough, and fever a few weeks ago.” Medical history is unremarkable, and the patient takes no medications. She has smoked a pack of cigarettes a day for the last 7 years, and smoked marijuana for a few months as a teenager. The patient is not sexually active and has never been pregnant. Her last menstrual period was 2 weeks ago. She is adopted, and her family history is unknown. Temperature is 38.3 C (100.9 F), blood pressure is 156/60 mm Hg, pulse is 110/min, and respirations are 22/min. The thyroid gland is diffusely enlarged, firm, and very tender. The extremities are warm and moist. Eye examination shows lid lag but no proptosis. The remainder of the examination is unremarkable. Laboratory results are as follows:
Hemoglobin
11 g/dL
Leukocytes
10,800/mm³
Aspartate aminotransferase (SGOT)
66 U/L
Alanine aminotransferase (SGPT)
70 U/L
Thyroid-stimulating hormone
<0.01 µU/mL
Thyroxine (T4), serum
18 µg/dL
Triiodothyronine (T3), serum
183 ng/dL
Erythrocyte sedimentation rate
90 mm/h
Item 1 of 2
A radioactive iodine uptake with scintigraphy in this patient is mostly likely to show which of the following?
CorrectIncorrect -
Question 20 of 40
20. Question
Item 2 of 2
Which of the following is the best treatment for this patient?
CorrectIncorrect -
Question 21 of 40
21. Question
A 28-year-old woman with type 1 diabetes mellitus comes to the office to discuss insulin management. She anticipates running in a 5-km (3.1-mile) race to raise money for diabetes research. The patient was diagnosed with type 1 diabetes mellitus 3 years ago and takes 24 units of insulin glargine at bedtime and 8 units of insulin lispro before meals. She is regimented with her meal timing (breakfast at 5:30 AM, lunch at noon, and dinner at 5:30 PM) and bedtime snack. Physical examination is unremarkable. Hemoglobin A1c is 6.9%. The race is scheduled to start at 6:30 AM. The patient expects that it will take her 30 minutes to complete it and plans to eat a high-fiber, high-carbohydrate snack afterward. She intends to have breakfast at her usual time of 5:30 AM on that day. Which of the following is the most appropriate adjustment in this patient’s insulin dose on the day of the race?
CorrectIncorrect -
Question 22 of 40
22. Question
A 76-year-old woman with a history of hypertension, type 2 diabetes mellitus, coronary artery disease, heart failure with preserved ejection fraction, and atrial fibrillation comes to the office for a follow-up visit. The patient says, “I feel exhausted all the time, and my feet are often swollen at the end of the day. I have also gained several pounds over the past 3 months.” She has had no chest pain, dyspnea, orthopnea, or dizziness. Her medications include low-dose aspirin, metoprolol, lisinopril, furosemide, metformin, insulin glargine, and a daily multivitamin supplement. The patient underwent electrical cardioversion for persistent atrial fibrillation 6 months ago and has since been taking amiodarone. Two months ago, anticoagulation was discontinued due to recurrent falls related to gait disturbance from diabetic neuropathy. Blood pressure is 134/70 mm Hg with no postural changes, pulse is 58/min and regular, and oxygen saturation is 96% on room air. Weight is 77 kg (170 lb), which is 4.5 kg (10 lb) more than her recorded weight a few months ago. With the head of the bed elevated to 30 degrees, the jugular venous pressure is 2 cm above the sternal angle. Hepatojugular reflux is absent. Lung fields are clear to auscultation. Trace edema is noted at the ankles. Decreased vibratory and light touch sensation is present in the distal lower extremities. The remainder of the physical examination is normal. Serum creatinine is 0.8 mg/dL, sodium is 132 mEq/L, and potassium is 3.7 mEq/L. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 34-year-old woman comes to the physician after several months of amenorrhea. Several home pregnancy tests have been negative. Her past medical history is insignificant. She is married with 2 children and has no plans to have more. Her body mass index is 23 kg/m2. Physical examination is unremarkable. Serum prolactin level is 500 ng/mL (normal 5-20 ng/mL). Magnetic resonance imaging of the head shows a 5-mm pituitary mass. This patient is at high risk of developing which of the following if left untreated?
CorrectIncorrect -
Question 24 of 40
24. Question
A 44-year-old male was found to have a fasting finger stick blood glucose level of 110 mg/dl. His fasting blood sugar levels were measured twice in the laboratory, and are 112 and 114 mg/dl, respectively. He denies any symptoms or past medical problems. He does not smoke or drink. He has a strong family history of diabetes mellitus. His physical examination, including weight and blood pressure, is unremarkable. His HDL cholesterol is 42 mg/dl and LDL cholesterol is 128 mg/dl. His HbA1c is 5.9%. Urinalysis is unremarkable. The findings described above put the patient at an increased risk of which of the following?
CorrectIncorrect -
Question 25 of 40
25. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to the Next Item, you will not be able to add or change an answer.
A 30-year-old woman comes to the office due to tiredness for the past 3 months. She has been unable to exercise due to excessive fatigue and muscle cramps. The patient has had no cold intolerance, constipation, or dry skin. She states, “My menstrual cycles have been unpredictable and very heavy.” Medical history is notable for episodic migraines, for which she began taking topiramate 6 months ago. The patient initially had significant weight loss after starting topiramate, but she has regained most of the weight over the last 2 months and continues to have occasional migraines. She also has a history of chronic anxiety and an episode of nephrolithiasis a few months ago. The patient lives alone, is not sexually active, and has had no pregnancies. She does not use tobacco, alcohol, or illicit drugs. The patient’s sister underwent a thyroidectomy for unknown reasons. Blood pressure is 136/80 mm Hg and pulse is 68/min. BMI is 28 kg/m2. The thyroid gland is normal in size and nontender. Deep tendon reflexes are normal; the remainder of the examination is unremarkable. Serum TSH is 5.7 µU/mL. Repeat TSH a month later is 5.6 µU/mL, and free T4 is normal.
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 26 of 40
26. Question
Item 2 of 2
Which of the following additional findings is most likely to be associated with this patient’s condition?
CorrectIncorrect -
Question 27 of 40
27. Question
A 58-year-old woman comes to the office for evaluation of excessive weight gain over the past 2 years despite a healthy diet and exercise. “I feel very tired and weak all the time no matter how much I sleep,” she reports. The patient has had particular difficulty climbing stairs. Medical history is significant for hypertension and type 2 diabetes mellitus. She reached menopause at age 48; she does not smoke cigarettes or drink alcohol. Blood pressure is 130/70 mm Hg and pulse is 88/min. BMI is 37 kg/m2. Physical examination shows that the patient has abdominal obesity and thin extremities. There is mild proximal weakness of the lower extremities. The result of 24-hour urinary cortisol measurement is more than 3 times the upper limit of normal. Late-night salivary cortisol level is significantly elevated. Plasma ACTH levels are undetectable. Which of the following is the best next diagnostic step in this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 42-year-old female complains of occasional nagging midabdominal pain. She describes the pain as crampy in quality and states that it is relieved by bowel movements. Sometimes the pain wakes her from sleep. She denies any associated nausea, vomiting, chest pain, fever or weight loss. She is otherwise healthy. Her blood pressure is 130/80 mmHg and her heart rate is 85/min. Physical examination is essentially unremarkable. Abdominal CT scan shows a right-sided adrenal mass measuring 2 cm in diameter. Which of the following is the best next step in managing this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
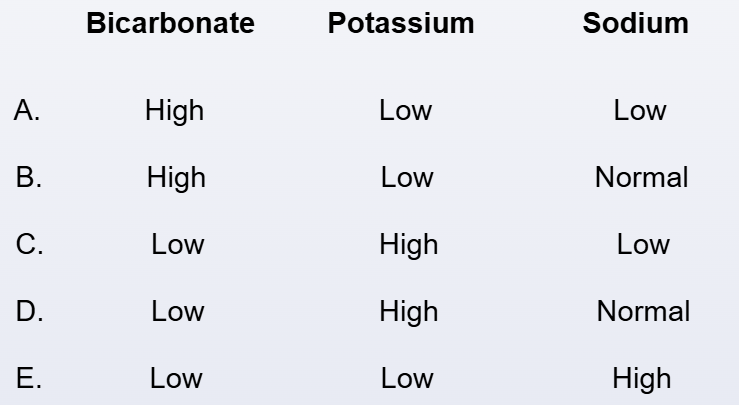
A 30-year-old woman comes to the office due to generalized weakness and paresthesia. Medical history is unremarkable, and she takes no medications. The patient mentions that her blood pressure was elevated at a workplace health fair 3 months ago; she attributed it to being “stressed out” and did not take any action. Blood pressure is 150/95 mm Hg. Cardiac examination is normal with full and symmetric distal pulses and no pedal edema. Laboratory evaluation shows low plasma renin activity and normal serum creatinine level. CT scan of the abdomen reveals a solitary, hypodense, 1.5-cm right adrenal mass. Which of the following patterns of serum electrolyte concentrations would most likely be seen in this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 30 of 40
30. Question
A 66-year-old man is found to have bilateral breast enlargement during a routine office visit. The patient reports no breast discomfort, headaches, or vision abnormalities but has had decreased libido and lack of energy for several months. Medical conditions include hypertension, hyperlipidemia, and osteoarthritis. The patient takes chlorthalidone, simvastatin, and acetaminophen as needed. He does not use over-the-counter or herbal supplements. The patient drinks 1 or 2 alcoholic beverages during social events and does not use tobacco or recreational drugs. He is married and has several adult children. Family history is notable for breast cancer in a maternal aunt. Vital signs are within normal limits. BMI is 32 kg/m2. Examination shows normal body hair distribution and no rashes. Breast examination demonstrates 2-cm, round, firm tissue behind the areolas bilaterally with no overlying skin changes or nipple discharge. There are no enlarged lymph nodes. External genitalia are normal in size and appearance, and no testicular masses are present. The remainder of the physical examination is normal. Laboratory results are as follows:
LH, serum
14 mU/mL (normal: 3-15)
Total testosterone, serum
310 ng/dL (normal: 300-1,200)
TSH
4.5 µU/mL (normal: 0.5-5)
Serum chemistry panel and liver aminotransferases are within normal limits, and serum testosterone level is unchanged on repeat testing. Which of the following is the most likely explanation for this patient’s breast abnormality?
CorrectIncorrect -
Question 31 of 40
31. Question
A 36-year-old woman comes to the office due to type 1 diabetes mellitus. She was initially diagnosed 20 years ago and is treated with a combination of long- and short-acting insulin analogues. A month ago, the patient had an episode of severe hypoglycemia with near loss of consciousness that required the administration of a home glucagon kit by her husband. Since then, she has felt normal. Review of the patient’s continuous glucose-monitoring system shows multiple glucose excursions <50 mg/dL in the past week; however, none of these episodes was associated with tremor, sweating, or altered mental status. Hemoglobin A1c is 7.8%. Which of the following interventions is most likely to restore hypoglycemic awareness in this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 50-year-old female was found to have abnormal thyroid function on routine blood testing. Her TSH level is 9 μU/ml (0.35 to 5.0 μU/ml is normal) and free T4 is 1.3 ng/dl (normal 0.8 to 1.8 ng/dl). She is currently asymptomatic and is taking no medications. She denies use of tobacco, alcohol, and drugs. Family history is positive for a mother with hypothyroidism. She has four siblings, all are alive and well. Her menstrual cycles are regular. Examination is unremarkable. Her CBC, serum chemistries, and lipid profile are within normal limits. Which of the following will be most useful in guiding her therapy?
CorrectIncorrect -
Question 33 of 40
33. Question
A 36-year-old woman comes to the office due to a 6-month history of lethargy and poor sleep. She has non-restorative sleep with frequent awakening throughout the night. The patient has also had a loss of appetite and decreased interest in day-to-day activities. In addition, she has had irregular menses, with infrequent, heavy, painless menstrual bleeding. There is no associated weight change, fever, cough, dyspnea, palpitations, abdominal pain, constipation, cold intolerance, or dry skin. Past medical history is unremarkable, and the patient takes no medications. She has a 10-pack-year smoking history, drinks alcohol socially, and does not use recreational drugs. Family history is positive for Graves disease in a sister and hypertension in her father. On examination, her blood pressure is 136/90 mm Hg, pulse is 78/min, and BMI is 27 kg/m2. The thyroid gland is diffusely enlarged and firm on palpation. Cardiopulmonary examination is normal, with no pedal edema. No focal neurological deficits are noted. Laboratory results show TSH of 9 μU/mL (normal 0.35-4.5 μU/mL), free T4 of 1.2 ng/dL (normal 0.8-1.8 ng/dL), and anti-thyroid peroxidase antibody present in high titers. Repeat TSH level is 8.8 μU/mL. Which of the following is the best next step in this patient’s care?
CorrectIncorrect -
Question 34 of 40
34. Question
A 37-year-old woman comes to the office for evaluation of fatigue and lower extremity edema for the past 3 weeks. She has had type 1 diabetes mellitus for 20 years. Current medications include basal and bolus insulin, atorvastatin, and lisinopril. Blood pressure is 158/90 mm Hg and pulse is 80/min. Examination shows 2+ bilateral pitting lower extremity edema and is otherwise normal. Laboratory results are as follows:
Hemoglobin A1c
6.9%
Serum albumin
3.1 g/dL
Serum creatinine
1.6 mg/dL
eGFR
38 mL/min/1.73 m2
Urinalysis
3+ protein
Urine albumin/creatinine ratio
3,500 mg/g
At her last office visit six months ago, serum creatinine was 1.1 mg/dL, eGFR was 64 mL/min/1.73 m2, and urine albumin/creatinine ratio was 500 mg/g. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 35 of 40
35. Question
A 59-year-old woman comes to the clinic due to a 2-month history of fatigue, myalgias, and bone pains. She has also experienced a 4.5-kg (10-lb) weight gain over the past year, which she attributes to physical inactivity and changes in her diet since immigrating to New York City from India to live with her son. Medical history is notable for alpha-thalassemia-1 trait, and the patient experienced menopause at age 49. She takes no medications or supplements. Vital signs are normal. BMI is 32 kg/m2. Physical examination is unremarkable. Laboratory results are as follows:
Hemoglobin
11 g/dL
Red cell distribution width
12% (12%-16%)
Basic metabolic panel
normal
TSH
2.3 U/L
Erythrocyte sedimentation rate
12 mm/hr
Creatine kinase
60 U/L
Which of the following is the most appropriate next step?
CorrectIncorrect -
Question 36 of 40
36. Question
A 52-year-old woman comes to the office for follow-up of long-standing primary hypothyroidism, which has been treated for the past 6 years with a stable dose of levothyroxine 0.125 mg. The patient is very compliant and takes her medication an hour before breakfast every day. Recently, however, she has had increasing weight gain, dry skin, cold intolerance, and lethargy. The patient otherwise feels well and experienced menopause 6 months ago. Laboratory results at that time showed a low serum 25-hydroxyvitamin D level, which improved with oral vitamin D supplementation. She is currently taking over-the-counter calcium and vitamin D supplements every morning with breakfast. Medical history is unremarkable, and family history is positive for osteoporosis in her mother. The patient has a 35-pack-year history of smoking but quit 3 months ago with bupropion as she heard that “smoking increases the risk of bone fractures.” She does not use alcohol or illicit drugs. Vital signs and physical examination are normal. Serum TSH is 9 μU/mL; it was 2.3 μU/mL a year ago. Complete blood count and basic chemistry profile are normal. Which of the following is the most appropriate advice for this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
A 23-year-old woman comes to the office due to recurrent hypoglycemia. The patient has a 6-year history of type 1 diabetes mellitus that has been treated with a stable dose of insulin in a basal-bolus regimen. However, for the last 3 months, she has had frequent episodes of hypoglycemia distributed evenly throughout the day; she has also had fatigue, loss of appetite, amenorrhea, and a 2-kg (4.4-lb) weight loss. The patient has had no change in activity and has experienced no fever or gastrointestinal, genitourinary, or respiratory symptoms. She is not sexually active and does not use tobacco, alcohol, or recreational drugs. Blood pressure is 90/60 mm Hg and pulse is 100/min. BMI is 20 kg/m2. Physical examination is unremarkable. Laboratory results are as follows:
Complete blood count
Hematocrit
38%
Platelet count
280,000/mm3
Leukocyte count
5,500/mm3
Segmented neutrophils
47%
Eosinophils
7%
Lymphocytes
40%
Monocytes
6%
Serum chemistry
Sodium
135 mEq/L
Potassium
5.6 mEq/L
Chloride
104 mEq/L
Bicarbonate
17 mEq/L
Blood urea nitrogen
30 mg/dL
Creatinine
1.2 mg/dL
Calcium
9.0 mg/dL
Glucose
45 mg/dL
Hemoglobin A1c
5.5 % (normal: 4%-6%)
TSH
4.0 μU/mL
ECG and urinalysis are unremarkable. In addition to decreasing the patient’s insulin dose, which of the following is the most appropriate course of action in management of this patient?
CorrectIncorrect -
Question 38 of 40
38. Question
A 36-year-old man comes to the office after he was found to have an abnormal lipid panel during employee wellness testing at his company. He has no prior medical problems and takes no medications. The patient is a software technician and has a sedentary lifestyle. He eats mostly fast foods, rarely exercises, and drinks 2-3 cans of beer daily. His BMI is 31 kg/m2. Physical examination is unremarkable. Results of laboratory studies performed in the office are as follows:
Total cholesterol 290 mg/dL High-density lipoprotein 45 mg/dL Low-density lipoprotein 110 mg/dL Triglycerides 675 mg/dL Lifestyle modification with a balanced diet, regular exercise, and reduced alcohol intake is advised. He is also started on fenofibrate therapy. This medication is most likely to help the patient by which of the following mechanisms?
CorrectIncorrect -
Question 39 of 40
39. Question
A 26-year-old woman, gravida 1 para 0, at 16 weeks gestation comes to the clinic for follow-up prenatal care. She was diagnosed with Graves disease during her first trimester and was treated with propylthiouracil, which was changed to methimazole 3 weeks ago. The patient has gained 7 kg (15.4 lb) over the last 4 months. She also has experienced increasing fatigue and states, “My breasts feel very full.” The patient has had no palpitations or shortness of breath, but her sleep has been interrupted by frequent urination. Her mother has hypothyroidism, which is treated with levothyroxine. The patient has never used tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 112/72 mm Hg, pulse is 90/min and regular, and respirations are 18/min. No murmurs are heard on cardiac auscultation. Thyroid examination shows mild, diffuse enlargement with no tenderness or bruit. Deep tendon reflexes are brisk but symmetrical. The remainder of the physical examination is normal. Thyroid function test results are as follows:
TSH
0.1 µU/mL (trimester-specific reference range: 0.2-3.0)
Serum T4 (total)
19 µg/dL (trimester-specific reference range: 7.5-18)
Serum T3 (total)
288 ng/dL (trimester-specific reference range: 105-285)
Which of the following is the most appropriate management for this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 65-year-old man comes to the emergency department due to a 2-week history of progressive dyspnea. The patient has been sleeping in a chair for the last 3 days because he cannot lie flat. Medical history includes hypertension, nonalcoholic steatohepatitis, myocardial infarction 6 years ago, and type 2 diabetes mellitus. He is taking a multidrug regimen for diabetes mellitus due to preference for avoiding insulin and minimizing cost. Current medications include metformin, glipizide, pioglitazone, aspirin, atorvastatin, metoprolol, and losartan. He is a lifelong nonsmoker. Blood pressure is 151/82 mm Hg, pulse is 72/min, and oxygen saturation is 92% on room air. Heart rate is regular, and an S3 is present on cardiac auscultation. Bilateral crackles are heard on chest examination. There is 2+ symmetric bilateral pitting edema. ECG shows normal sinus rhythm. Cardiac enzymes are negative, and renal and hepatic function studies are normal. Chest x-ray reveals increased interstitial markings with Kerley B lines and small bilateral pleural effusions. Which of the following medications most likely contributed to this patient’s current condition?
CorrectIncorrect
