Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 3 items
A previously healthy 28-year-old Caucasian woman comes to the physician because of fatigue, arthralgias, and chest pain over the past 6 months. She has had a 2.3-kg (5-lb) weight loss during this period. She denies any recent travel or sick contacts. Her past medical history is insignificant. She takes no medications and has no known drug allergies. She is sexually active and uses condoms for contraception. She has never been pregnant. She does not use tobacco, alcohol, or drugs. Her mother has rheumatoid arthritis. Her temperature is 37.2 C (99 F), blood pressure is 122/77 mm Hg, and pulse is 78/min. Physical examination shows a faint facial rash. The lungs are clear to auscultation with mildly decreased breath sounds at the left lung base. The abdomen is soft and non-tender. There is no organomegaly. There is no peripheral edema. Neurologic examination is unremarkable.
Item 1 of 3
Which of the following tests is most likely to be positive in this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 3
Further evaluation reveals a positive antinuclear antibody (ANA) screen in high titers. Other lab studies show:
WBC
3,200/mm3
Hemoglobin
10.2 g/dL
Platelets
87,000/mm3
Which of the following antibody titers is most likely to correlate with the disease activity in this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
Item 3 of 3
The patient returns one week after the initial visit. Her laboratory work-up shows the following additional findings:
Anti-dsDNA antibodies positive ESR 44 mm/hr Serum creatinine 0.8 mg/dL Total bilirubin 0.8 mg/dL Aspartate aminotransferase (AST) 32 U/L Alanine aminotransferase (ALT) 22 U/L Alkaline phosphatase 86 U/L Urinalysis Protein none WBC 5-10/hpf RBC 0-2/hpf An x-ray film of the chest shows a mild, left-sided pleural effusion. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 4 of 40
4. Question
The following vignette applies to the next 2 items.
A 55-year-old woman comes to the physician due to a 2-month history of malaise, mild fever, and difficulty climbing stairs and rising from a chair. She has unintentionally lost 9.1 kg (20.1 lb) over this period. The patient has hypertension and asthma. Medications include amlodipine, as-needed albuterol, and inhaled glucocorticoids during winter. The patient does not smoke or use illicit drugs. She worked for 20 years supervising cotton processing in a textile factory but has been working as a secretary for the past 10 years. Temperature is 37.8 C (100 F), blood pressure is 120/70 mm Hg, pulse is 82/min, and respirations are 12/min. Chest examination reveals clear lung fields and normal S1 and S2. The patient has bilateral proximal upper and lower extremity weakness with normal reflexes. Plantar reflexes are down-going bilaterally. Violaceous papules and plaques are seen on the dorsum of both hands, as shown in the image below:

Kidney and liver function are within normal limits. Creatine kinase level is 1,200 IU/L.
Item 1 of 2
Which of the following is the best next step in management of this patient?CorrectIncorrect -
Question 5 of 40
5. Question
Item 2 of 2
Which of the following conditions is most likely associated with this patient’s disease?CorrectIncorrect -
Question 6 of 40
6. Question
A 29-year-old woman comes to the office due to 3 months of worsening exertional dyspnea and nonproductive cough. The patient says, “I thought the symptoms were from a cold or allergies, but they have not gone away and have gotten worse. None of the over-the-counter congestion medicines from the pharmacy have helped.” She has also had occasional joint pain and has felt too tired to keep up with her exercise routine of running 5 miles 3 times a week. She has had no chest pain, palpitations, syncope, or leg edema. The patient has no chronic medical problems and does not use tobacco, alcohol, or illicit drugs. Her brother has asthma. Laboratory results are as follows:
Complete blood count
Hemoglobin
12.8 g/dL
Platelets
320,000/mm3
Leukocytes
9,000/mm3
Serum chemistry
Sodium
142 mEq/L
Potassium
4.2 mEq/L
Bicarbonate
26 mEq/L
Blood urea nitrogen
18 mg/dL
Creatinine
0.9 mg/dL
Calcium
11.2 mg/dL
Glucose
86 mg/dL
Erythrocyte sedimentation rate
55 mm/hr
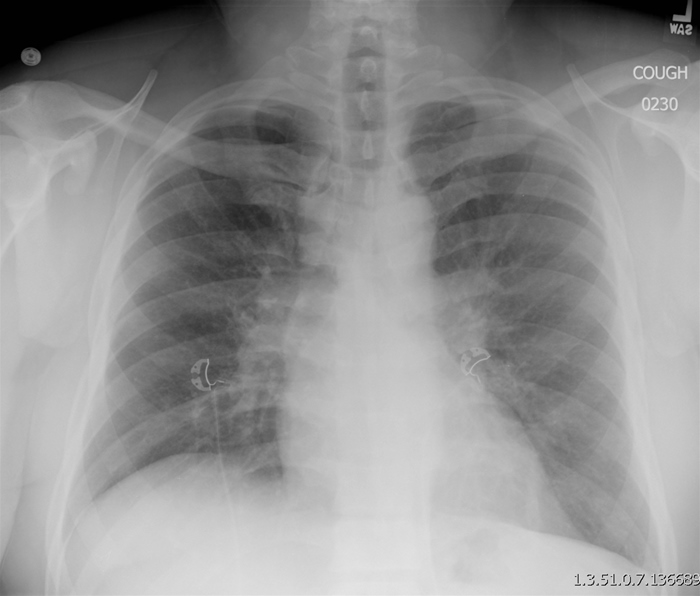
Chest radiography is shown in the exhibit. Pulmonary function testing reveals that FEV1 is 60% of the predicted value, FEV1/FVC is 80%, and diffusion capacity for carbon monoxide is 60% of predicted. After discussion of a likely diagnosis and possible therapy, the patient asks about long-term prognosis. Which of the following is the most appropriate response to this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 7 of 40
7. Question
A 70-year-old man comes to the office due to pain and stiffness of his neck, shoulders, and hips for the past 3 months. The stiffness is worse in the morning and lasts 1-2 hours. He also has had general malaise and a recent weight loss of 3.17 kg (7 lb). The patient has no headache, scalp tenderness, visual symptoms, or jaw claudication. Examination shows no overt synovitis at the joints, with normal passive range of motion. The arteries of the scalp, neck, and extremities are normal on palpation without any tenderness. Laboratory results are as follows:
Leukocytes
7,500/µL
Hematocrit
31%
Platelets
450,000/µL
Erythrocyte sedimentation rate
85 mm/h
TSH
1.8 µU/mL
Creatine kinase
33 U/L
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
A 73-year-old man comes to the office due to pain and restriction of movement in his left hip joint for the last 6 months. He has been taking over-the-counter acetaminophen 2-3 times a day, although this does not give any significant relief from this pain. His medical history is significant for type 2 diabetes mellitus and hypertension. He is currently on metformin, hydrochlorothiazide, and atenolol. His father has hypertension and gout. He has a 30-pack-year history of smoking, but he quit smoking 10 years ago. He has a history of alcohol abuse during his early 20s. Currently, he drinks a glass of wine over the weekends. Physical examination reveals restricted movement in his left hip joint, with pain on passive flexion. The rest of the physical examination is unremarkable. X-ray of his left hip joint and pelvis reveals thickening of outer cortex of his left proximal femur with mild bowing. Sclerotic lesions are also present on the left ischial bone. Technetium bone scan shows an increased uptake in the frontal bone, left scapula, left ischium, and whole of his left proximal femur. A basic metabolic profile, including calcium and creatinine levels, is unremarkable. What is the most appropriate treatment for this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
The following vignette applies to the next 2 items.
A 48-year-old woman comes to the office due to a 1-week history of a lump in her neck. She has muscle pains and body aches. Upon further questioning, she adds that she often experiences a “gritty, burning sensation in both of my eyes, and sometimes they get red and inflamed.” She does not wear contact lenses. She has not had fever, chills, weight loss, dysphagia, cough, hemoptysis, muscle weakness, or joint swelling. Medical history includes fibromyalgia, depression, and cholelithiasis. She has extensive caries of her teeth and has been visiting a dentist regularly. She does not use tobacco, alcohol, or drugs. Her only medication is fluoxetine. Temperature is 37.0 C (98.6 F), blood pressure is 122/80 mm Hg, pulse is 76/min, and respirations are 14/min. BMI is 27 kg/m2. Examination shows a mobile, non-tender 2×2 cm right-sided submandibular mass.
Item 1 of 2
Which of the following is the most appropriate next step to confirm the underlying diagnosis in this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
Item 2 of 2
The appropriate test is suggestive of the diagnosis, and a Schirmer test confirms inadequate tear production in this patient. Which of the following is the most likely explanation for this patient’s neck mass?
CorrectIncorrect -
Question 11 of 40
11. Question
A 52-year-old woman comes to the emergency department (ED) on a Saturday night with severe low back pain. She has a history of chronic back pain, for which her pain management physician prescribes oxycodone. However, the patient’s pain has become worse recently, and her normal dose of oxycodone has not been effective. She is very angry because she called her physician’s office multiple times before finally reaching the covering physician, who directed her to go to the ED. The patient requests that the emergency physician prescribe a stronger pain medication and says, “Now that I took all the trouble to come to the emergency department, I better get some relief!” She has no prior history of visits to this ED, and no medical records are available. Which of the following is the most appropriate reaction to the patient’s request?
CorrectIncorrect -
Question 12 of 40
12. Question
A 43-year-old man comes to the office for follow-up regarding back pain. Three weeks ago, the patient had acute-onset pain in the low back radiating to the buttocks after lifting heavy bags of fertilizer at his farm. The patient was treated with naproxen; with treatment, the pain has decreased from 8/10 to 3/10 in severity and no longer radiates. Medical history is notable only for 2 prior episodes of back pain in the last year. Vital signs are normal. BMI is 33 kg/m2. Physical examination shows no spinal tenderness, normal lower extremity strength and reflexes, and a negative straight-leg raising test bilaterally. The patient asks what is needed to prevent future episodes of back pain. Which of the following is the most appropriate response to this patient’s question?
CorrectIncorrect -
Question 13 of 40
13. Question
A 46-year-old nurse comes to the acute care clinic 3 weeks after injuring her left knee while transferring a patient. She felt a “twinge,” but there was no immediate deformity or subsequent edema, and she was able to continue walking normally. Within 2 weeks, she developed intense pain around the left knee and could hardly walk or put any weight on the left leg. Placing clothing or sheets on the left knee produces abnormal discomfort and insomnia. She is prescribed naproxen and oxycodone. Over the next 2 months, the patient notes swelling around her left knee, an increased temperature, and more sweating of the left leg compared to the right. Sometimes the left leg has a mottled, bluish discoloration. Even on analgesics, exacerbation of her knee pain by flexion and extension causes her to limp. She also complains of poor sleep and constant fatigue. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 14 of 40
14. Question
The following vignette applies to the next 2 items
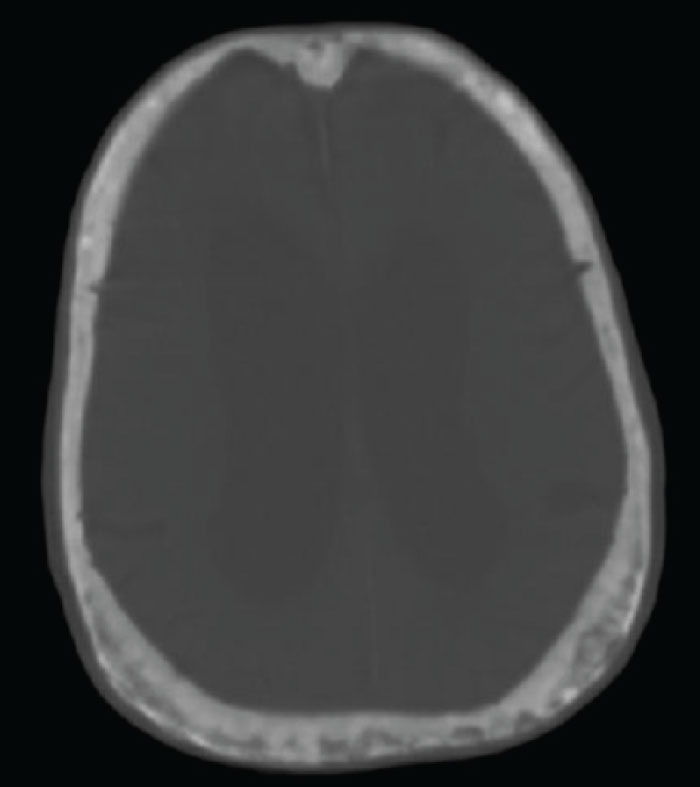
A 66-year-old man comes to a community clinic after undergoing a computed tomography scan of the head at a local emergency department. He fell while stepping out of the bathtub and struck his head but did not lose consciousness. The patient sustained a small head laceration that was closed with sutures, but no other injuries were identified in the emergency department. He reports a longstanding history of normal-pressure hydrocephalus with frequent falls, but he has not followed up with his neurologist for several years. The patient is now asymptomatic with no headaches, focal weakness, or dizziness. His head computed tomography scan with bone windows is shown in the image below.
Item 1 of 2
What is the best next step in management of this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
Item 2 of 2
After the appropriate steps, the patient returns for follow-up one year later. He now complains of hearing loss in the left ear. What is the appropriate response to his complaint?
CorrectIncorrect -
Question 16 of 40
16. Question
The following vignette applies to the next 2 items.
A 46-year-old woman comes to the office for follow-up of rheumatoid arthritis. The patient was diagnosed 2 years ago and started on treatment with prednisone and methotrexate; she had a good initial response to treatment, and the oral glucocorticoid was gradually tapered. However, her symptoms have progressively worsened over the last several months, despite increases in the methotrexate dose. The patient continues to have hand stiffness and pain lasting 2-3 hours every morning and increasing knee and ankle pain. She takes frequent doses of acetaminophen and ibuprofen but her symptoms still significantly restrict her daily activities. Medical history is otherwise unremarkable. The patient does not use tobacco, alcohol, or illicit drugs. Physical examination shows symmetric swelling and tenderness of the proximal small hand joints, wrists, and knees. Blood cell count shows mild normochromic, normocytic anemia with normal leukocyte and platelet counts. Erythrocyte sedimentation rate is 55 mm/hr. Hand x-ray reveals periarticular osteopenia and mild joint erosions.
Item 1 of 2
After discussion of treatment options, tumor necrosis factor inhibitor therapy is planned. Which of the following tests is most appropriate prior to beginning the treatment?
CorrectIncorrect -
Question 17 of 40
17. Question
Item 2 of 2
The new treatment is initiated and the patient’s symptoms gradually improve. Six months later, she returns to the office with 12 hours of right knee pain. The patient has had no trauma and says, “This pain is more severe than prior arthritis flare-ups.” Temperature is 38.3 C (101 F), blood pressure is 130/80 mm Hg, pulse is 82/min, and respirations are 14/min. Right knee examination demonstrates a moderate effusion, warmth, and tenderness. Range of motion is decreased due to pain. Which of the following is the best next step in management of this patient’s condition?
CorrectIncorrect -
Question 18 of 40
18. Question
The following vignette applies to the next 2 items. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 48-year-old man comes to the office due to progressive weakness for the past 2 months. The patient has experienced difficulty climbing stairs, especially when carrying heavy items such as groceries, and his symptoms have become progressively worse. He also reports occasional fevers, but no significant pain in the muscles or joints. The patient has had no diplopia, dyspnea, dysphagia, abdominal pain, or heat or cold intolerance. He has a history of hypertension and hyperlipidemia, for which he has taken losartan and atorvastatin, respectively, for the last 4 years. The patient does not use tobacco, alcohol, or illicit drugs. Temperature is 37.1 C (98.8 F), blood pressure is 132/84 mm Hg, pulse is 72/min, and respirations are 14/min. He has no scleral icterus. Cardiopulmonary examination is normal. The abdomen is soft and nontender with no hepatosplenomegaly. Muscle strength is 3/5 in the deltoids and hip flexors but is otherwise normal. Deep tendon reflexes are normal and symmetric, and sensations to pain and light touch are intact. There is mild muscle tenderness and some of the small joints of both hands are tender to palpation without any swelling or erythema. He has no skin rash. Laboratory results are as follows:
Complete blood count
Hemoglobin
13.3 g/dL
Platelets
305,000/mm3
Leukocytes
9,800/mm3
Serum chemistry
Blood urea nitrogen
14 mg/dL
Creatinine
0.9 mg/dL
Glucose
140 mg/dL
Liver function studies
Alkaline phosphatase
66 U/L
Aspartate aminotransferase
312 U/L
Alanine aminotransferase
214 U/L
TSH
7.2 µU/mL
Thyroxine (T4), serum
6.1 µg/dL
Creatine kinase, serum
4200 U/L
C-reactive protein
12.6 mg/L (<8 mg/L)
Erythrocyte sedimentation rate
38 mm/h
Item 1 of 2
Which of the following is the most likely cause of this patient’s current symptoms?
CorrectIncorrect -
Question 19 of 40
19. Question
Item 2 of 2
After confirmation of the diagnosis, the patient is started on appropriate therapy. During a follow-up visit 6 months later, he says the muscle weakness has improved but he becomes breathless on moderate exertion. The patient has to stop to catch his breath when walking 3 blocks to his office, which he had previously been able to do without stopping. He has also had a mild nonproductive cough. Temperature is 36.6 C (98 F), blood pressure is 130/80 mm Hg, pulse is 82/min, and respirations are 16/min. The neck veins are flat. Heart sounds are normal, but lung auscultation reveals bibasilar fine crackles. Muscle strength is normal. Blood cell counts and serum chemistry are within normal limits. Chest radiograph is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 62-year-old woman comes to the office due to a 3-month history of painful, swollen wrists and knees. She also has joint stiffness, which is worse upon wakening and limits her daily activities. Review of systems is positive for fatigue. The patient’s only other medical condition is hypothyroidism for which she takes levothyroxine. She smoked a pack of cigarettes daily for 20 years and quit 15 years ago. Vitals signs are within normal limits. Physical examination shows symmetric, moderate swelling of the wrists and knees. The joints are tender and warm. Range of motion is intact but painful. Plain radiographs of the symptomatic joints show joint space narrowing and marginal erosions. Which of the following cytokines are primarily involved in the pathogenesis of this patient’s joint destruction?
CorrectIncorrect -
Question 21 of 40
21. Question
A 65-year-old woman comes to the office due to osteoporosis that was recently diagnosed from a screening DXA scan. She feels well, eats a balanced diet, and gets regular exercise. Medical history is unremarkable, but family history includes osteoporosis in the patient’s mother and sister. Vital signs and physical examination are normal. Results from complete blood count and serum chemistry panel are normal. DXA revealed a T-score of −2.7 at the lumbar spine. The patient says, “I’m interested in taking alendronate to prevent fractures. My sister takes it, and it keeps her osteoporosis from getting worse.” Which of the following tests should be performed prior to prescribing this medication?
CorrectIncorrect -
Question 22 of 40
22. Question
The following vignette applies to the next 2 items
A 50-year-old obese man comes to the emergency department with toe pain. He awoke this morning with sudden severe pain in his left great toe. He has never had this type of pain before and has had no trauma to the toe. The patient has a history of hypertension treated with hydrochlorothiazide. He also has osteoarthritis in his right knee that was treated with an intraarticular steroid injection 6 months ago. He smokes a pack of cigarettes and drinks 1 or 2 glasses of wine daily. His temperature is 36.7 C (98.1 F), blood pressure is 130/80 mm Hg, pulse is 88/min, and respirations are 12/min. The patient’s left great toe is inflamed, with swelling and erythema at the metatarsophalangeal joint. There is pain with minimal range of motion. There are no skin rashes. The remainder of the examination is within normal limits.
Item 1 of 2
Which of the following is the best next step in confirming the diagnosis?
CorrectIncorrect -
Question 23 of 40
23. Question
Item 2 of 2
The diagnosis of acute gout is made. Which of the following is the preferred treatment for the patient at this time?
CorrectIncorrect -
Question 24 of 40
24. Question
A 38-year-old woman comes to the office due to abdominal pain. For the last 2-3 weeks, she has had increasingly severe abdominal pain associated with watery diarrhea. The patient has a history of Crohn disease treated for the last year with adalimumab, which has controlled the symptoms until now. Vital signs are normal except for a temperature of 37.8 C (100 F). Examination shows moderate tenderness in the right lower quadrant with no peritoneal signs. Laboratory results show an undetectable trough adalimumab level. Which of the following is the most likely explanation for this patient’s worsening symptoms?
CorrectIncorrect -
Question 25 of 40
25. Question
A married couple comes to the office for routine prenatal counseling. The husband is 120 cm (3 ft 11 in) tall with disproportionately short upper and lower extremities, a large head, and a prominent forehead. He cannot provide a biological family history because he was adopted. His spouse is average height with no dysmorphic features, and her family history is insignificant. They inquire about the likelihood that their offspring will have short stature due to the same condition as the father. Which of the following is the best response to their concerns?
CorrectIncorrect -
Question 26 of 40
26. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 27-year-old woman comes to the office due to pain in her left knee, ankle, and lower back that started a week ago. The patient says that her back feels stiff in the morning and “loosens up” with activity. She has had no pain in the small joints of her hands or feet. She reports no prior joint pain, recent flu-like symptoms, or trauma. Six months ago, a Chlamydia trachomatis infection was diagnosed at an urgent care center. She took doxycycline and currently has no genitourinary symptoms. The patient has no other medical conditions, and her only medication is an oral contraceptive pill. She is sexually active with multiple partners. Vital signs are normal. Physical examination shows a mild left knee effusion and tenderness without erythema or warmth. The left ankle is tender but not swollen or red. Other joints are normal on examination. No rash is present. Leukocyte count is 8,200/mm3, and erythrocyte sedimentation rate is 80 mm/hr. Synovial fluid aspirated from the knee has a white blood cell count of 4,000/mm3 with 80% neutrophils. Gram stain and polarized microscopy demonstrate no abnormalities.
Item 1 of 2
Which of the following is the best next step in diagnosing the cause of this patient’s joint pain?
CorrectIncorrect -
Question 27 of 40
27. Question
Item 2 of 2
Nucleic acid amplification testing of vaginal fluid is positive for Chlamydia trachomatis and negative for Neisseria gonorrhoeae. Tests for other sexually transmitted infections are ordered. In addition to antimicrobial therapy for the patient and her partner and as-needed nonsteroidal anti-inflammatory drug therapy for the joint pain, which of the following interventions is most appropriate at this time?
CorrectIncorrect -
Question 28 of 40
28. Question
The following vignette applies to the next 5 items
A 26-year-old Italian-American man comes to your office for the evaluation of low back pain. He has had this pain for the last eight months, and it is progressively getting worse. The pain is worse in the morning and gets better as the day progresses. He denies any history of trauma in the past. He works as a chef at a local restaurant. His father and uncles also have “back problems.” His physical examination reveals a limited range of motion of his lumbosacral spine and markedly reduced chest expansion. The rest of his physical and musculoskeletal examination is unremarkable.
Item 1 of 5
Which of the following is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
Item 2 of 5
If the initial evaluation shows mild disease, what would you do to monitor the disease activity?
CorrectIncorrect -
Question 30 of 40
30. Question
Item 3 of 5
Which of the following conditions is associated with the patient’s diagnosis?
CorrectIncorrect -
Question 31 of 40
31. Question
Item 4 of 5
The patient is given a prescription for non-steroidal anti-inflammatory agents. He returns for a follow-up visit after two weeks, and says that he feels a lot better. His pain and stiffness have almost resolved with daily intake of medications. He used to swim and exercise regularly before his symptoms developed a few months ago, and he wants to resume these activities, but he is concerned that his disease may get worse if he does so. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 32 of 40
32. Question
Item 5 of 5
Which of the following is the most appropriate statement regarding the prognosis of this condition?
CorrectIncorrect -
Question 33 of 40
33. Question
The following vignette applies to the next 2 items.
A 45-year-old man comes to the office due to pain and stiffness in his left shoulder for the past 3 months. His symptoms were mild and intermittent at first but have worsened in the past month and are now constant throughout the day and night. The pain is worse with lying on the shoulder. The patient is a professional painter and has had no acute injury. Medical history includes type 1 diabetes mellitus. Examination of the left shoulder shows no focal tenderness with global restriction in all directions with both active and passive range of motion. The right shoulder joint has normal range of motion. The remainder of the physical examination is normal. X-ray of the left shoulder is unremarkable.
Item 1 of 2
Which of the following is the most likely cause of this patient’s shoulder pain?CorrectIncorrect -
Question 34 of 40
34. Question
Item 2 of 2
An appropriate diagnosis is made after the patient is evaluated. Which of the following is the best next step in management of this patient?CorrectIncorrect -
Question 35 of 40
35. Question
A 60-year-old man comes to the physician for preoperative evaluation prior to right total knee replacement. He continues to smoke half a pack of cigarettes daily and has a 25-pack-year history. He reports mild shortness of breath when walking 4 blocks and up 2 flights of stairs and thinks that his dyspnea may have progressed slowly over the past 2 years. He uses a cane and admits to walking slowly due to knee pain. The patient has never been hospitalized but he gets bronchitis every winter that usually responds well to rescue albuterol. He was diagnosed with asthma and mild emphysema 4 years ago and takes tiotropium and fluticasone/salmeterol daily. His other medical problems include hypertension, degenerative joint disease, and anemia. The patient takes hydrochlorothiazide and as-needed tramadol for pain. His temperature is 36.7 C (98 F), blood pressure is 120/76 mm Hg, pulse is 80/min, and respirations are 16/min and unlabored. Oxygen saturation is 95% on room air. General physical examination (including lung examination) is unremarkable.
Laboratory study results are as follows:
Hemoglobin 12.6 g/dL Platelets 200,000 /µL Sodium 142 mEq/L Potassium 4.0 mEq/L Chloride 108 mEq/L Bicarbonate 26 mEq/L Blood urea nitrogen 14 mg/dL Creatinine 0.8 mg/dL Albumin 4.0 g/dL Which of the following additional studies should be performed to make an appropriate risk assessment prior to the planned surgery?
CorrectIncorrect -
Question 36 of 40
36. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 36-year-old woman comes to the emergency department due to a severe, throbbing headache that began several hours ago. She also has acute onset of blurred vision and nausea. She took acetaminophen, which did not provide any relief. The patient was diagnosed with Raynaud phenomenon a few years ago. She recently started having heartburn, for which she takes over-the-counter famotidine. Temperature is 36.7 C (98 F), blood pressure is 200/110 mm Hg, and pulse is 94/min. Pulse oximetry shows 94% in room air. There is no abdominal bruit. Ophthalmologic examination demonstrates bilateral papilledema. Laboratory results are as follows:
Complete blood count
Hemoglobin
11.5 g/dL
Mean corpuscular volume
82 µm3
Platelets
280,000/mm3
Leukocytes
7,500/mm3
Serum chemistry
Sodium
135 mEq/L
Potassium
4.2 mEq/L
Chloride
98 mEq/L
Bicarbonate
20 mEq/L
Blood urea nitrogen
30 mg/dL
Creatinine
2.0 mg/dL
Calcium
9.0 mg/dL
Glucose
120 mg/dL
Item 1 of 2
All her routine laboratory values were completely normal 6 months ago. Her blood pressure during her previous visits was always <120/80 mm Hg. What is the most likely diagnosis of this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
Item 2 of 2
Which of the following is the most appropriate pharmacotherapy?
CorrectIncorrect -
Question 38 of 40
38. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 36-year-old man comes to the emergency department due to acute pain in his left foot. He was previously feeling well but suddenly woke from sleep with severe pain at the base of his great toe. The patient has type 1 diabetes mellitus complicated by peripheral sensory neuropathy and proliferative retinopathy. He also has end-stage renal disease due to diabetic nephropathy, for which he underwent cadaveric renal transplant 18 months ago. The patient’s diabetes is controlled by an insulin pump. His other medications include lisinopril, amlodipine, cyclosporine, mycophenolate, and prednisone (5 mg/day). Temperature is 37.3 C (99.1 F), blood pressure is 126/84 mm Hg, and pulse is 88/min. Physical examination shows an erythematous, swollen, warm, and tender left first metatarsophalangeal joint. Range of motion testing is limited by severe pain. There is a moderate hammertoe deformity at the third toe but no abnormal calluses. Posterior tibial and dorsalis pedis pulses are easily palpable. Bedside capillary glucose is 184 mg/dL.
Item 1 of 2
Aspiration of the affected joint is likely to reveal which of the following in this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
Item 2 of 2
Examination of joint aspirate confirms the presence of crystals. Leukocyte count in the synovial fluid is 30,000/mm3. Gram stain is negative for organisms. Which of the following is the most appropriate drug for management of acute monoarthritis in this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 35-year-old man comes to the office due to joint pain. The patient is a charter pilot and operates flights from Wisconsin to the Caribbean islands, where he frequently stays for several weeks. During his most recent trip 3 months ago, he had fever and malaise for several days accompanied by severe pain in his fingers, wrists, and ankles. Since then, he has had persistent joint pain that has slightly improved over time. The patient has no fever, night sweats, rash, or abdominal symptoms. He is also an avid hiker. Temperature is 37 C (98.6 F), blood pressure is 130/72 mm Hg, and pulse is 80/min. No scleral icterus, mucosal lesions, or lymphadenopathy is present. The lungs are clear on auscultation, and there are no heart murmurs. The abdomen is soft and nontender with no hepatosplenomegaly. Tenderness and mild swelling are noted in the bilateral wrists, metacarpophalangeal joints, and ankles. No rash is present. Blood cell counts and serum chemistry study results are within normal limits. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect
