Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 3 items
An 18-year-old man comes to the physician for daytime sleepiness lasting several months. The patient recently started college, has difficulty staying awake during classes, and often falls asleep suddenly even though he “gets a good night’s sleep.” He typically goes to bed at 2 am and sleeps until at least 9 am, usually later. The patient’s sleep pattern at night is fragmented. He wakes frequently but is usually able to go back to sleep within a few minutes. He does not snore or wake up gasping. The patient feels like “someone is in the room with me when I’m just falling asleep and I sometimes hear my name being called.” His past medical history is otherwise insignificant. The patient does not use tobacco or alcohol. Blood pressure is 120/70 mm Hg and heart rate is 70/min. His body mass index is 23 kg/m2.
Item 1 of 3
Which of the following is the best next step in diagnosing the cause of this patient’s symptoms?
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 3
Which of the following is the best initial therapy for this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
Item 3 of 3
The appropriate treatment is initiated, but the patient returns in 4 weeks and says that his symptoms have not improved. He recently had “some little troubles” in his family, and has felt sudden onset of muscle weakness and falls, especially during arguments with his family members. What is the best next step in management of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
A 50-year-old woman comes to the office due to a 6-month history of periodic involuntary closure of her right eye. The closure is provoked by bright light or cigarette smoke. The patient reports no other abnormal movements involving the head, limbs, or trunk. Medical history is significant for osteoarthritis of her left knee. She takes naproxen occasionally. Vital signs are normal. An attempt to check the pupillary reaction induces prolonged closure of the right eye. Otherwise, the neurologic examination is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 5 of 40
5. Question
The following vignette applies to the next 2 items.
A 12-year-old boy is brought to the emergency department due to unsteadiness, weakness, and falls. The patient recently went on a week-long family camping and hiking trip to the mountains in Washington State. On returning home to California 2 days ago, he experienced a sense of fatigue and a tingling sensation in his fingers. Yesterday, the patient started having bilateral leg weakness and is now unable to walk without assistance; he sways from side to side when standing and then falls to the floor. The patient has had no fever, headache, joint pain, or skin rash and has no history of recent respiratory or gastrointestinal illness. Vital signs are within normal limits. He is alert and active but can stand only briefly before requiring assistance. There is no increased resistance to neck flexion. Cranial nerve examination is normal and sensation is not impaired. Muscle strength is 4/5 in the upper extremities and 2/5 in the lower extremities. Deep tendon reflexes are absent at the knees and ankles but are normal elsewhere. Finger-to-nose testing shows dysmetria of the arms.
Item 1 of 2
Which of the following is the best next diagnostic intervention that should be performed for this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
Item 2 of 2
Diagnostic intervention reveals significant findings. Which of the following is most likely to improve this patient’s condition?
CorrectIncorrect -
Question 7 of 40
7. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 56-year-old man is hospitalized due to a 7-hour history of left-sided weakness and difficulty speaking. Medical history is significant for hypertension and type 2 diabetes mellitus. He smokes 1.5 packs of cigarettes daily and consumes alcohol occasionally. Medications include antihypertensives and oral antidiabetic medications. Blood pressure is 185/111 mm Hg and pulse is 90/min. Physical examination shows left-sided hemiplegia with hemisensory loss and mild dysarthria. Cardiac auscultation demonstrates a regular rhythm without murmurs or additional sounds. There are no carotid bruits. Finger-stick glucose is 184 mg/dL. ECG shows left ventricular hypertrophy with secondary repolarization changes. CT scan of the head without contrast reveals focal hypodensity involving the right posterior limb of the internal capsule. CT angiography of the head and neck reveals no large vessel occlusion.
Item 1 of 2
Which of the following interventions is most appropriate at present?CorrectIncorrect -
Question 8 of 40
8. Question
Item 2 of 2
Swallow evaluation shows that the patient has normal swallowing capabilities, and he is given aspirin orally. Five hours after hospital admission, the neurologic examination remains unchanged. Blood pressure is now 175/95 mm Hg and heart rate is 98/min. Laboratory results are as follows:Hemoglobin
14.1 g/dL
Platelets
220,000/mm3
Creatinine
0.8 mg/dL
INR
1.1 (normal: 0.8-1.1)
Finger-stick glucose is 138 mg/dL. Which of the following pharmacotherapies is indicated for this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 78-year-old man is brought to the office by his daughter, who states that he has become forgetful. Over the past year, his responses have become slow, and he has had increasing difficulties in caring for himself. He was recently seen by another physician, who suspected a “certain type of anemia.” He has no urinary or respiratory problems. The patient was previously diagnosed with hypertension and coronary artery disease. He takes lisinopril, metoprolol, and aspirin. He lives with his daughter and son-in-law. He does not use tobacco, alcohol, or illicit drugs. Examination shows an elderly man who is disoriented to time and place and communicates poorly. He speaks softly and slowly and seems to think too much about his answers. The mini-mental state examination (MMSE) score is 22 points (normal >24). The patient’s gait is slow and cautious, as if he were expecting to fall. Laboratory test results are as follows:
Complete blood count
Hematocrit
41%
Mean corpuscular volume (MCV)
104 fL
Leukocytes
8,000/µL
Segmented neutrophils
65%
Lymphocytes
35%
Platelets
280,000/µL
Serum chemistry
Sodium
130 mEq/L
Potassium
4.1 mEq/L
Chloride
94 mEq/L
Bicarbonate
26 mEq/L
Blood urea nitrogen
16 mg/dL
Creatinine
0.8 mg/dL
Calcium
9.6 mg/dL
Glucose
96 mg/dL
Vitamin B12
400 pg/mL
Which of the following is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
A 42-year-old woman comes to the office due to 6 months of worsening headaches. The patient has had occasional headaches in the past, but lately “they seem to be getting out of control” and are often throbbing. She also has constant, pressure-like headaches localized behind the forehead and eyes. The patient takes acetaminophen and ibuprofen and recently began taking them on a daily basis. The medications often make her nauseated, and she has had several episodes of vomiting. The patient also has blurry vision but no muscle weakness, syncope, or seizures. She experiences a considerable amount of stress at work and says that she “cannot afford to slow down.” Medical history is significant for irritable bowel syndrome and chronic back pain. She smokes a pack of cigarettes daily. The patient’s mother suffered from migraines and had surgery for a meningioma. Her father died of a drug overdose. Blood pressure is 155/98 mm Hg and pulse is 83/min. BMI is 27 kg/m2. Chest examination is unremarkable. Abdominal examination shows mild periumbilical tenderness. There is no muscle weakness, and the deep tendon reflexes are symmetric. There is no hand tremor. Romberg test is negative. Funduscopic findings are shown in the image below.
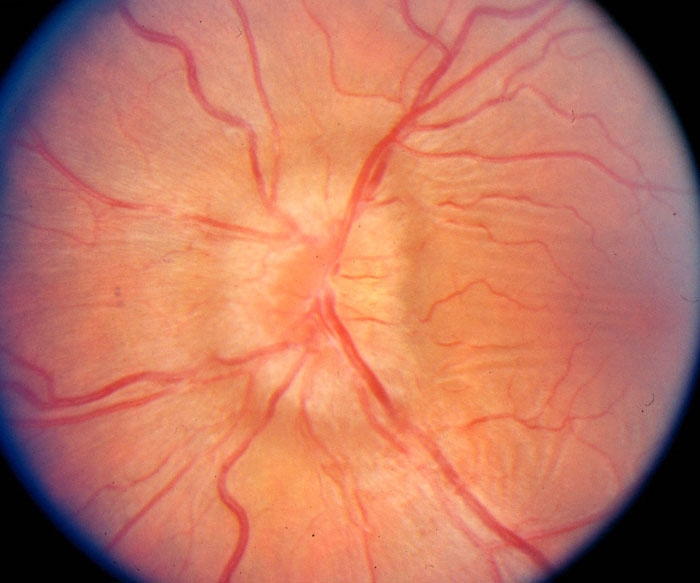
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 38-year-old man is brought to the emergency department after his family found him unresponsive at his home. He has a history of T6 paraplegia due to traumatic spinal cord injury 2 years ago and major depression. Emergency medical personnel found the patient with a pulse but no respirations and intubated him at the scene. Several empty bottles of diazepam and baclofen were found nearby. On arrival at the hospital, temperature is 36.2 C (97.2 F), blood pressure is 110/68 mm Hg, and pulse is 66/min. Neurologic examination shows fixed and dilated pupils. Cranial nerve and biceps reflexes are absent. There is no upper extremity withdrawal from pain. Cardiopulmonary examination is normal. Laboratory testing shows normal blood cell counts, serum electrolytes and glucose, liver aminotransferases levels, and arterial blood gases. No ethanol, acetaminophen, or salicylate is detected in the serum. Urine toxicology screen is positive for benzodiazepines. CT scan of the head is normal. The patient is admitted to the intensive care unit and supportive care is provided. Over the next 24 hours, he remains comatose with an unchanged neurologic examination. Electroencephalography reveals a burst suppression pattern consistent with global cerebral dysfunction but no epileptiform activity. Which of the following best applies to this patient?
CorrectIncorrect -
Question 12 of 40
12. Question
The following vignette applies to the next 2 items.
A 34-year-old man comes to the office due to an abnormal sensation over his right thigh. He says, “It gets numb, and, sometimes, I feel burning over my thigh.” He has no back pain, muscle weakness, or abnormal sensation below the knee. Medical history is insignificant. He smokes 2 packs of cigarettes and consumes 1 or 2 bottles of beer daily. He is a construction worker and frequently works in a squatting position. Vitals signs are normal. BMI is 37 kg/m2. Physical examination reveals an area of decreased sensation over the right anterolateral thigh. There is no muscle weakness. Deep tendon reflexes are symmetric.
Item 1 of 2
Which of the following is the most likely cause of this patient’s condition?CorrectIncorrect -
Question 13 of 40
13. Question
Item 2 of 2
Which of the following is the most appropriate next step in management of this patient?CorrectIncorrect -
Question 14 of 40
14. Question
A 26-year-old man comes to the emergency department with a 3-day history of dull back pain, progressive difficulty in walking, and urinary retention. He had a mild upper respiratory infection one week ago, but he is otherwise healthy. He is not taking any medications and denies recreational substance use. Temperature is 36.7 C (98 F), blood pressure is 120/76 mm Hg, pulse is 80/min, and respirations are 16/min. Neurologic examination reveals a decreased muscle strength (2/5) bilaterally in the lower extremities, hyporeactive knee and ankle reflexes, and decreased pain sensation up to the umbilical level. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 15 of 40
15. Question
A 65-year-old man is brought to the office by his daughter due to decreased activity and impaired sleep over the past month. He was diagnosed with Parkinson disease 2 years ago. According to his daughter, he displays very few emotions and does not want to do anything. She says, “He has been slowing down these past few years and I suppose that was to be expected, but I am worried that he’s getting worse so quickly. He just sits in his chair and watches TV with a blank expression. He has been waking up early in the morning, which is very unusual for him. When I suggest that he should go out, he says he is too tired or makes excuses. It’s like he doesn’t care much about anything.” The patient is quiet during most of the discussion. He does not disagree with his daughter’s comments, but says, “I’m alright. I manage. I don’t have much to add.” The patient is adherent with his current levodopa/carbidopa treatment. His other medication is pravastatin for hypercholesterolemia. He does not use tobacco, alcohol, or illicit drugs. Physical examination shows masklike facies and slowed movements. Mild hand tremor and postural instability have improved since his last visit. Which of the following is the most appropriate next step in pharmacological management of this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
A 27-year-old man comes to the office due to progressively worsening headaches and vision changes for the past 3 months. For the past 2 weeks, he has had increasing nausea with some vomiting. The patient has no motor weakness or sensory symptoms. On physical examination, his pupils do not react to light bilaterally. The patient has an impaired upward gaze and retraction of the upper eyelids. The rest of his eye movements are within normal limits. He has bilateral papilledema. The physical examination is otherwise unremarkable. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 17 of 40
17. Question
A 24-year-old man comes to the office due to facial weakness. Over the past day, his face has become droopy on the right side. Two months ago, after the patient returned from hiking in the northern Appalachian Mountains, he had an illness with fatigue, headache, and an annular rash that resolved in a week without treatment. He has no other medical conditions. On examination, there is no rash. Extraocular movements are intact; the conjunctivae are clear. The external auditory canals are normal, and the tympanic membranes are clear and mobile. The face is symmetric at rest, but there is weakness on the right side with voluntary movement. The right eyebrow does not raise as high as the left, the right eye does not close fully, and the right side of the mouth does not elevate to match the left. Which of the following is the most appropriate next step in this patient?
CorrectIncorrect -
Question 18 of 40
18. Question
A 38-year-old man comes to the office due to difficulty with public speaking. He is a college professor and regularly gives hour-long lectures to students. Over the past 4-5 months, the patient has had spasms of his jaw when speaking. His jaw will move to the right and clench very tightly, which is quite painful and renders him unable to speak. Previously, sometimes the symptoms would resolve when the patient placed his water bottle on the right side of his cheek, which would immediately stop the spasm. However, the symptoms have been getting worse, which caused him to cancel 2 lectures in the past month. Vital signs are normal. Physical examination including neurologic examination is normal. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 19 of 40
19. Question
A 36-year-old man has had weakness in his right arm and leg as well as difficulty walking over the past 2 weeks. This was preceded for several days by mild headaches and dizziness that have not recurred. He is an ex-smoker with a 10-pack-year history. The patient experimented with cocaine in college although never intravenously, and he has used no illicit drugs in the last 10 years. He has a history of multiple sexual partners and has been treated twice in the past several years for gonococcal urethritis. He also reports an ulcerative lesion on his penis “a while ago,” that resolved. The patient has no history of diabetes or hypertension. His family history is negative for stroke or premature coronary artery disease. He is afebrile, his blood pressure is 132/80 mm Hg, and his heart rate is 85/min with a regular rhythm. There is no murmur on cardiac examination. His reflexes are hyperactive on the right side. Electrocardiogram shows normal sinus rhythm. A urine toxicology screen is negative. Brain MRI demonstrates a subacute stroke in the left frontal lobe. HIV test is negative. Cerebrospinal fluid analysis results are as follows:
Red blood cells 2/mm3 Leukocytes 215/mm3 Lymphocytes 95% Protein 165 mg/dL Glucose 58 mg/dL Cerebrospinal fluid Gram stain shows no organisms. Which of the following is most likely to indicate the underlying etiology of this patient’s symptoms?
CorrectIncorrect -
Question 20 of 40
20. Question
A 30-year-old man comes to the office due to burning pain and numbness in the first three digits of his right hand. These symptoms woke him last night. He is a baker and rolls dough using repetitive movements, including hyperextension of the wrist and pronation of the forearm. He remembers having several similar episodes of finger numbness that resolved completely after a period of rest. Medical history is otherwise insignificant. Which of the following is the most likely localization of the pathologic process in this patient?
CorrectIncorrect -
Question 21 of 40
21. Question
A 55-year-old woman comes to the emergency department with progressively worsening severe back pain and difficulty walking for the last 2 weeks. The pain is at the mid-thoracic level and wraps around her upper abdomen in a band-like fashion. She also has weakness, numbness, and tingling in both lower extremities. No bowel or bladder dysfunction is reported. The patient completed treatment for non-Hodgkin’s lymphoma 8 months ago with chemotherapy and radiation therapy. On physical examination, her temperature is 36.7 C (98 F), blood pressure is 110/80 mm Hg, and pulse is 94/min. Neurological examination shows motor strength of 3/5 in both lower extremities. The patellar and Achilles reflexes are brisk and Babinski reflex is upgoing bilaterally. Which of the following are the most appropriate next steps in management of this patient?
CorrectIncorrect -
Question 22 of 40
22. Question
The following vignette applies to the next 2 items
A 45-year-old Caucasian man comes to see you in the office. He is accompanied by his wife. They have noticed that he has shakiness of both hands for the past six months. The shakiness is limited only to his hands and has not progressed over time. It becomes much more pronounced when he tries to pick up things or attempts to eat or drink. On physical examination, you notice a constant tremor in both his hands, which becomes much more pronounced when his arms are outstretched. There is also a very subtle head tremor present. There is no rigidity or slowing of voluntary movements in the upper or lower extremities. His father had a similar problem in his 50s or 60s, but he is not sure what treatment he received at that time. His wife is extremely anxious and wants to know his prognosis.
Item 1 of 2
Which of the following is the most appropriate response?
CorrectIncorrect -
Question 23 of 40
23. Question
Item 2 of 2
The patient works as a carpenter and feels that he is unable to perform the fine motor tasks due to the tremor. Which of the following is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
A 45-year-old woman comes to the emergency department due to sudden-onset, severe headache. On arrival, the patient is alert and oriented and has no focal neurological deficits. CT scan of the head reveals subarachnoid hemorrhage, and she is admitted to the critical care unit. Over the next several hours, the patient gradually becomes somnolent and less responsive. She opens her eyes to painful stimuli only and does not follow commands. Repeat imaging of the brain shows no new hemorrhage, but there is enlargement of the entire ventricular system compared to the previous CT scan. Which of the following is the most likely cause of this patient’s neurologic deterioration in the hospital?
CorrectIncorrect -
Question 25 of 40
25. Question
A 28-year-old man comes to the emergency department in the middle of the night due to unrelenting headache. The patient was awakened 2 hours before by severe, sharp periorbital pain on the left side of his head. He also has had nausea and watering from the left eye. The patient took ibuprofen and acetaminophen but experienced no relief. About 3 months ago, he had similar headaches over the course of several days that resolved spontaneously. Temperature is 37 C (98.6 F), blood pressure is 140/90 mm Hg, pulse is 92/min, and respirations are 16/min. Pulse oximetry shows 98% on ambient air. The patient appears to be in pain and is restless. Physical examination shows mild ptosis and miosis of the left eye. There is clear discharge from the left nostril. The patient has no other focal neurologic deficits, and the remainder of the physical examination is normal. Which of the following is the most appropriate intervention at this time?
CorrectIncorrect -
Question 26 of 40
26. Question
A 14-year-old girl with a history of juvenile myoclonic epilepsy is brought to the emergency department after 2 generalized tonic-clonic seizures that started approximately 1 hour ago. She has not returned to baseline between seizures. The patient was prescribed daily levetiracetam, but her parents suspect that she has not taken it for the past week. On arrival, the airway is patent, and she has good respiratory effort. Blood pressure is 123/82 mm Hg, pulse is 130/min, respirations are 16/min, and pulse oximetry shows 99% on 2 L oxygen via nasal cannula. The patient’s eyes are open, but she is not responding to commands. Neurologic examination shows pupils that are equal but minimally responsive to light. Intermittent twitching of the mouth, both arms, and both legs is observed. Fingerstick glucose is 115 mg/dL. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
The following vignette applies to the next 3 items.
A 24-year-old man is brought to the emergency department by his girlfriend due to progressive weakness. They have been on a cross-country road trip for the past month. While traveling through the midwestern United States 2 weeks ago, the patient developed diarrhea, nausea, and vomiting. He rested, drank fluids, and improved spontaneously after 2-3 days. However, the patient had persistent fatigue, and 4 days ago they had to stop traveling as his legs became too weak to press down the brake pedal. He is now unable to get out of bed. The patient has also had tingling of the hands and feet as well as shortness of breath. He has had no fever, chills, abdominal pain, or recurrent diarrhea. The patient has no prior medical problems and takes no medications. He does not use tobacco, alcohol, or illicit drugs. Temperature is 37.7 C (99.8 F), blood pressure is 120/70 mm Hg, pulse is 90/min, and respirations are 20/min. Pulse oximetry shows 98% on ambient air. The patient is awake, alert, and speaking in full sentences but develops a weak cough after taking a sip of water. The lungs are clear to auscultation and heart sounds are normal. The abdomen is soft and nontender. Neurologic examination shows symmetric bilateral lower extremity weakness. Deep tendon reflexes are absent at the knees and ankles, and 1+ in the biceps and triceps. Cranial nerve examination and sensation are normal, and he has no neck rigidity. There is no skin rash or lymphadenopathy.
Item 1 of 3
Which of the following is the best immediate step in management of this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
Item 2 of 3
Which of the following is the best treatment modality for this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
Item 3 of 3
The patient is told that the diarrheal illness may have triggered his current condition, and he becomes upset that he did not seek medical attention earlier. He inquires about the course and prognosis of his current condition. Which of the following is the most accurate statement?
CorrectIncorrect -
Question 30 of 40
30. Question
A 75-year-old woman is brought to the office by her son for evaluation of worsening forgetfulness over the past few years. She has had difficulty remembering names of the people she meets and frequently misplaces household items. Recently, the patient forgot to turn off the stove after cooking but had no major fire. She has also had disrupted sleep with frequent awakenings throughout the night. Vital signs are within normal limits. On physical examination, the patient is alert and cooperative but disoriented to time and can recall only 1 of 3 items on a short-term memory test. MRI of the head reveals diffuse cortical atrophy. A medication with which of the following effects would be most beneficial for this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 36-year-old woman comes to the office with her mother for evaluation of abnormal movements for the past 5 months. The patient has been physically restless and clumsy, dropping objects frequently. She was previously traveling across South America as a photographer for a magazine but had to stop working a month ago due to “shaky hands.” Family medical history includes depression in the patient’s father, who died in a motor vehicle collision a few years after her birth. Medical history is noncontributory. Vital signs are normal. The patient is alert and fully oriented. Intermittent facial twitching and asymmetric, jerking movements of the upper extremities are noted. She is unable to protrude her tongue for a sustained period of time. Muscle strength and tone are normal. Gait is normal. She recalls 1 of 5 objects after 5 minutes. Which of the following is the most likely clinical course for this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 56-year-old man is brought to the emergency department due to prolonged generalized seizures for 30 minutes. The patient has alcohol use disorder and previous alcohol withdrawal seizures. He is intubated to secure the airway. Serum sodium is 118 mEq/L. The seizures terminate with intravenous lorazepam and hypertonic saline infusion. On hospital day 11, the patient remains on the ventilator with no spontaneous respirations or limb movements despite sedation being stopped 7 days ago. Temperature is 37.5 C (99.5 F), blood pressure is 129/77 mm Hg, pulse is 80/min, and ventilator respiratory rate is 16/min with no patient-triggered breaths. The patient’s eyes are mostly closed at night and intermittently open during the day. Pupillary light reflexes are normal bilaterally. He blinks on command but has no withdrawal of extremities to pain. Repeat serum chemistry and complete blood count are normal. CT scan of the head shows moderate generalized cerebral volume loss. Nerve conduction velocity and muscle potentials are normal. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 33 of 40
33. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 55-year-old man comes to the emergency department 2 hours after the onset of weakness in his left arm and leg. Two months ago, the patient had a 15-minute episode of right arm weakness that resolved spontaneously. He has no headache, nausea, vomiting, or difficulty swallowing. Temperature is 36.7 C (98.1 F), blood pressure is 172/98 mm Hg, and pulse is 83/min with a regular rhythm. Physical examination shows left-sided hemiparesis. Finger-stick blood glucose is 108 mg/dL. CT scan of the head without contrast reveals no signs of intracranial hemorrhage. The patient is given thrombolytic therapy. CT angiography of the head and neck reveals no large-vessel occlusion and no significant arterial stenosis. The next day, neurologic examination shows marked improvement in left-sided weakness. Carotid duplex ultrasound reveals 20% stenosis of the right internal carotid artery and 30% stenosis of the left internal carotid; there is no evidence of thrombosis or ulceration. ECG shows normal sinus rhythm. Complete blood count and coagulation studies are normal.
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?CorrectIncorrect -
Question 34 of 40
34. Question
Item 2 of 2
MRI of the head reveals a cortical infarct in the right middle cerebral artery territory. Echocardiography reveals left ventricular hypertrophy with an ejection fraction of 60% and moderate left atrial dilation. There are no valvular lesions, wall motion abnormalities, intracardiac thrombi, or intracardiac shunts. A small (1 mm) atheroma is present in the aortic arch without ulceration. The patient is observed in the hospital for 48 hours on the telemetry floor; there is no evidence of arrhythmia. Serum erythrocyte sedimentation rate is normal and rapid plasma reagin is negative. Which of the following is the most appropriate next step in management of this patient?CorrectIncorrect -
Question 35 of 40
35. Question
A 63-year-old man comes to the emergency department due to sharp, stabbing pain on the right side of the face and hiccups that started 6 hours ago. The patient is right-handed and has been unable to feed himself since his symptoms started. He has a history of stable angina, hypertension, and hyperlipidemia. Medications include atenolol, simvastatin, and aspirin. Vital signs are within normal limits. The patient has horizontal and vertical nystagmus and ptosis of the right eye. Gag reflex is diminished. He reports loss of pain and temperature sensation on the right side of the face and left trunk and limbs, as well as severe dizziness when attempting to stand. Which of the following is the most likely location of this patient’s brain lesion?
CorrectIncorrect -
Question 36 of 40
36. Question
A 44-year-old man comes to the office due to paresthesia and pain in his feet. The patient began experiencing tingling and numbness in his toes several months ago, which gradually progressed to the rest of both feet. He has also had burning pain on the soles, which frequently disrupts his sleep at night. The patient has a 6-year history of HIV infection. He was not adherent to treatment initially but now takes antiretroviral therapy regularly. His most recent CD4 cell count was 550/mm3. Vital signs are within normal limits. Foot examination shows decreased pain and touch sensation and loss of ankle reflexes bilaterally. There are no other focal neurologic deficits. Medication review shows no neurotoxic drugs and laboratory studies are within normal limits. Treatment with duloxetine is planned. This medication is most likely to improve this patient’s symptoms via which of the following mechanisms?
CorrectIncorrect -
Question 37 of 40
37. Question
A 56-year-old woman is brought to the emergency department due to several days of progressive dyspnea, productive cough, and fever. Today, her son found her very short of breath and obtunded. The patient has a history of hypertension, type 2 diabetes mellitus, and long-standing rheumatoid arthritis. Examination reveals bilateral pneumonia and severe respiratory distress. The patient is lethargic without focal neurologic deficits. Urgent endotracheal intubation is performed for mechanical ventilation, and the patient is started on broad-spectrum antibiotics. Repeat examination 2 hours later shows that she has developed areflexic, flaccid paralysis of all extremities. Which of the following is the most likely cause of the neurologic deficits in this patient?
CorrectIncorrect -
Question 38 of 40
38. Question
A 60-year-old man comes to the office due to a “shaking” of his right hand for several months. The patient says that it is worse while watching TV but that he frequently forgets about it while working or doing his regular daily activities. He works as an accountant, and his writing has become smaller; he has difficulty buttoning clothes and tying shoelaces. Medical history is significant for recurrent episodes of major depression, and he has been taking sertraline. The patient’s father died of a hemorrhagic stroke at age 80. Temperature is 37 C (98.6 F), blood pressure is 125/68 mm Hg in both arms, and pulse is 72/min. BMI is 27 kg/m2. Physical examination shows a tremor in the patient’s right hand that diminishes with movement and involuntary resistance to flexion of the right wrist and right arm. Hand opening and closing, as well as finger tapping, are slow. No sensory abnormalities are present. Muscle strength is preserved on both sides. Plantar reflexes are flexor bilaterally. What is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 65-year-old woman comes to the office due to progressive difficulty with walking for the past year. In addition, the patient has difficulty lifting her right leg to get into and out of a car, getting dressed using the right arm, turning over in bed, and peeling vegetables, especially with the right hand. Examination shows lack of facial expression, cogwheel rigidity in all extremities, a shuffling gait, and a fine resting tremor of the right hand. In addition to levodopa, carbidopa is also started, mainly to reduce the severity of the adverse effects of levodopa. Which of the following adverse effects is most likely to persist despite adding carbidopa to the patient’s treatment regimen?
CorrectIncorrect -
Question 40 of 40
40. Question
A 62-year-old man comes to the office with his wife due to behavioral changes. The patient has become increasingly impulsive and irritable over the past 1-2 years. He recently lost his job after making inappropriate comments and touching female coworkers. The patient has also lost interest in his hobbies and appears withdrawn during social gatherings. His other medical problems are hypertension and hyperlipidemia. A thorough neuropsychological assessment is conducted. Inability to perform which of the following tasks would be most indicative of frontal lobe dysfunction?
CorrectIncorrect
