Time limit: 0
Quiz Summary
0 of 15 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 15 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 15
1. Question
A 12-year-old boy is brought to the emergency department with right eye pain after being hit by a tennis ball an hour ago. His eye was closed when the ball hit it. The patient reports pain and blurry vision in the right eye but no headache, neck pain, or loss of consciousness. He has no chronic medical conditions and takes no medications. Vital signs are normal. On examination, there is mild periorbital soft tissue swelling and bruising around the right eye. There is no proptosis. The right pupil has a normal shape, but there is layering of blood in the anterior chamber that covers more than half of the right pupil. Extraocular movements are intact. There is no bony tenderness of the orbit or other facial bones. Visual acuity is 20/40 in the right eye and 20/20 in the left eye. In addition to appropriate pain control, which of the following is the best immediate next step in management of this patient?
CorrectIncorrect -
Question 2 of 15
2. Question
A 35-year-old man is brought to the emergency department due to severe left eye pain. A few hours earlier, when he was working on his boat, he dropped a heavy metal crate onto the boat’s wooden deck and immediately felt one or more small foreign objects enter his left eye. The eye began to water profusely, and the patient has been unable to open it to examine it sufficiently. He does not wear contact lenses and has no medical conditions. Examination of the left eye reveals conjunctival hyperemia with a few small debris on the surface of the eye. The pupil is round and reactive to light, and the anterior chamber is clear. Visual acuity is normal. Upon staining the left eye with fluorescein and visualizing it with a slit lamp, multiple vertical parallel lines of fluorescein uptake are seen in the upper quadrant of the cornea. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 3 of 15
3. Question
A 45-year-old African-American woman presents to the emergency department with the complaint that “my eye hurts, and it’s far too bright in here.” She has one hand cupped over her left eye. She denies any history of trauma or the presence of a foreign body sensation in either eye. Physical examination reveals significant redness at the junction between the cornea and sclera of the left eye. The left pupil is irregular and constricted and she recoils when the penlight is shined in either eye. Visual acuity is reduced in the left eye. Slit lamp examination shows the presence of leukocytes in the anterior segment of this eye. What is the cause of this woman’s symptoms?
CorrectIncorrect -
Question 4 of 15
4. Question
A 58-year-old airline captain comes to the office after he was found to have abnormal vision testing during a pilot medical certification examination. The patient feels well and has no ocular symptoms. Vision testing shows normal visual acuity but moderate loss of peripheral vision in both eyes. Results of the funduscopic examination are shown in the image below.
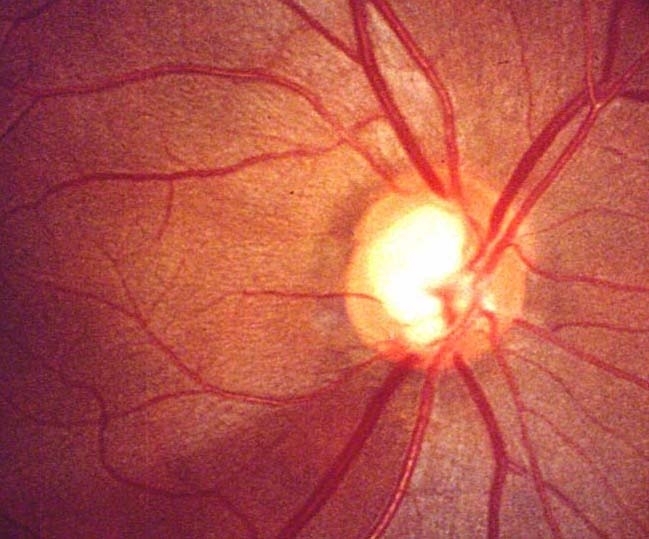
Other neurologic and cardiopulmonary examination findings are unremarkable. He is started on latanoprost eyedrops. The medication is most likely to improve this patient’s condition through which of the following mechanisms?
CorrectIncorrect -
Question 5 of 15
5. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 63-year-old man with a history of locoregionally advanced squamous cell carcinoma of the oropharynx is admitted to the hospital due to cancer-related pain of the mouth and throat. The pain has slowly worsened over the last several days and has limited his ability to eat and drink. The patient has felt weak and believes he is dehydrated. He was diagnosed with cancer 4 months ago and has received several cycles of chemotherapy and radiation therapy, the last of which occurred a week ago. The patient has been told that his tumor is unresectable. On admission, temperature is 36.1 C (97 F), blood pressure is 105/60 mm Hg, pulse is 108/min, and respirations are 12/min. BMI is 17 kg/m2. Physical examination shows periorbital wasting, dry mucous membranes, and sloughing of the oral mucosa. Absolute neutrophil count is 350/mm3. The patient is admitted to a medical floor and given intravenous analgesics; total parenteral nutrition is initiated via a central venous catheter. On day 7 of hospitalization, he has a temperature of 39.1 C (102.4 F) and new right eye pain and light sensitivity. Right eye visual acuity is decreased with a clear cornea and anterior chamber. Funduscopic examination reveals vitreous haze and several large, glistening, off-white chorioretinal lesions with indistinct borders.
Item 1 of 2
What is the most likely cause of this patient’s ocular symptoms?CorrectIncorrect -
Question 6 of 15
6. Question
Item 2 of 2
Urgent ophthalmologic consultation is obtained. Which of the following is the best initial therapy for this patient?CorrectIncorrect -
Question 7 of 15
7. Question
A 78-year-old man is brought to the office due to recurrent falls. The patient is a nursing home resident, and the nursing home staff noticed that he has a progressive decrease in vision. The patient has not had any double vision, dizziness, nausea, vomiting, headache, or vertigo. Medical problems include Alzheimer dementia, peptic ulcer disease, diverticulosis, and degenerative joint disease. Vital signs are stable. On examination, he has decreased vision in both eyes, and bilateral anterior cortical cataracts. Which of the following associated conditions is most likely contributing to his decreased vision?
CorrectIncorrect -
Question 8 of 15
8. Question
A 75-year-old man comes to the office due to a 2-year history of slowly worsening vision in both eyes. The symptoms are worse at night and the patient has stopped driving at night due to excessive glare from oncoming headlights. He has worked his entire life as a farmer and continues to drive tractors and other farm equipment during the day without difficulty. Medical history is unremarkable. Ocular examination shows loss of the red reflex and poor visualization of retinal detail. Acuity testing shows 20/100 vision in both eyes; visual field testing is normal. Which of the following is the most likely etiologic factor for this patient’s eye condition?
CorrectIncorrect -
Question 9 of 15
9. Question
A 42-year-old man comes to the emergency department due to a week of eye pain and blurry vision. Initially, he developed mild red eye and irritation, which he attempted to manage with artificial tear drops. The patient works as a commercial fisherman and had assumed his symptoms were due to frequent sun and water exposure. However, over the past few days, his eye pain has worsened, and he can “barely see” out of his left eye. He has no medical history but has a family history of hypertension and diabetes. Temperature is 37.2 C (99.1 F). Blood pressure is 128/82 mm Hg, pulse is 70/min, and respirations are 11/min. There is copious clear drainage from the left eye, and a large ulceration is overlying the cornea; the right eye appears unremarkable. Minimal sensation of the left cornea is noted during esthesiometry testing. With fluorescein application, additional shallow linear, branched ulcerations are visualized along the margins of the central defect of the affected eye. Routine Gram stain of the bacterial culture shows numerous white blood cells but no organisms. Which of the following should be started immediately in this patient?
CorrectIncorrect -
Question 10 of 15
10. Question
A 65-year-old man comes to the office due to eye irritation for the past 4 months. The patient’s eyes have felt dry and “gritty.” The feeling is usually worse in the morning. Yesterday, he had difficulty opening his right eye because his eyelids felt stuck together. The patient has worn glasses for 50 years and has had no recent change in vision. On examination, both eyelids appear pink with some oily-appearing crusted flakes around the eyelashes. The eyelashes appear thinned, and some have no pigment. There is mild, diffuse conjunctival erythema. Extraocular movements are intact; pupillary light reflexes are normal. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 11 of 15
11. Question
A 45-year-old woman comes to the clinic due to blurry vision in the left eye. The patient first noticed some decreased visual acuity 2 days ago and thought she may need a new prescription for her glasses. However, the blurriness has progressively worsened. The patient has no eye pain or foreign body sensation and does not wear contact lenses. Temperature is 36.8 C (98.2 F), blood pressure is 110/78 mm Hg, pulse is 76/min, and respirations are 14/min. On examination, visual acuity is moderately reduced in the left eye. The upper and lower eyelids can fully open and close bilaterally. Corneal esthesiometry reveals decreased sensation of the left cornea. Fluorescein examination shows a large, geographic ulceration and several linear, branched defects overlying the cornea. Dysfunction in which of the following nerves is most likely the cause of this patient’s impaired corneal sensation?
CorrectIncorrect -
Question 12 of 15
12. Question
A 69-year-old man comes to the emergency department with 1 hour of sudden vision loss in his right eye. The patient has no headache, eye pain, itching, or discharge. He has a history of coronary artery disease, type 2 diabetes mellitus, hypertension, and hyperlipidemia. The patient was diagnosed with prostate cancer 6 months ago and treated with radiation therapy. Physical examination shows severely compromised vision in the right eye. He can recognize hand motion but cannot count fingers. Funduscopic findings are shown below.
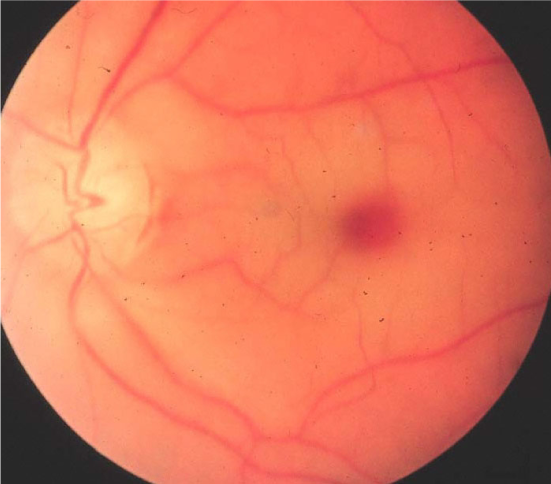
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 13 of 15
13. Question
A 29-year-old woman comes to the emergency department with left eye pain and redness. Three hours ago, her 9-month-old infant accidentally scratched her eye with his fingernail while she was rocking him to sleep. She washed her eye thoroughly with water but has continued to have eye pain and redness since. Vital signs are normal. On examination, the patient reflexively tries to keep her left eye closed, and excessive tearing is present. The conjunctiva of the left eye is erythematous; there is no obvious foreign body. The pupils are round, symmetric, and reactive to light; extraocular movements are intact. The eye is anesthetized with tetracaine, and fluorescein stain is applied. Slit-lamp examination reveals concentrated linear uptake of fluorescein with subsequent clearing in a waterfall pattern from the 9-o’clock position of the cornea. In addition to the appropriate pain control, which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 14 of 15
14. Question
A 20-year-old man with type 1 diabetes comes to the office due to blurry vision in both eyes for the past 7 days. The patient has difficulty reading television captions and seeing words on the board in the classroom. He has had no redness, discharge, or pain in his eyes. The patient also reports increased thirst and urination. He was diagnosed with diabetes mellitus a year ago and was prescribed a basal-bolus insulin regimen. The patient states that, lately, he has been unable to take insulin as prescribed due to busy class schedules. His most recent ophthalmology evaluation 3 months ago was unremarkable. Vital signs are normal. Physical examination shows normal extraocular movements and pupillary responses. There is no conjunctival edema or erythema. Visual acuity using a Snellen chart is 20/40 (normal: 20/20). Funduscopic examination appears grossly unremarkable. Bedside tonometry is normal. Point-of-care hemoglobin A1c is 9.0% and random blood glucose is 320 mg/dL. Which of the following is the most likely explanation for this patient’s visual changes?
CorrectIncorrect -
Question 15 of 15
15. Question
A 50-year-old woman with type 2 diabetes mellitus, hypertension, and obesity comes to the emergency department with left-sided vision loss that started 45 minutes ago. She has no fever, headache, eye pain, or tearing. On examination, she can only see hand motion with her left eye and cannot count fingers. Visual acuity in the right eye is normal. Funduscopic findings are shown below.
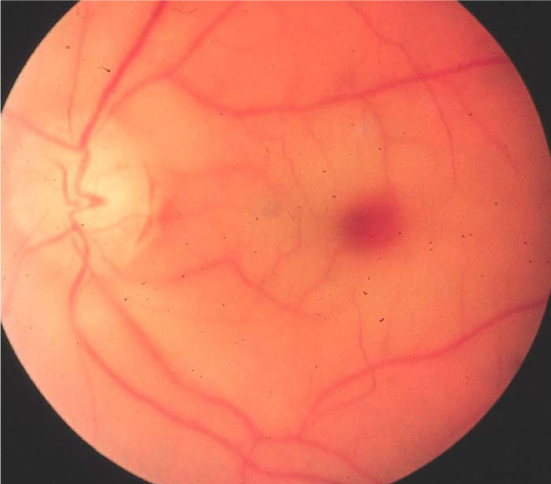
Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect
