Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 9-year-old boy is brought to the office by his parents due to knee pain. His mother states, “His left knee has been intermittently painful and swollen for approximately 2 weeks, but it’s gotten a lot worse over the past 5 days.” The patient plays basketball but has had no recent trauma to the knee area. He has had no fever, headaches, or chest pain. The patient recalls a tick bite 3 months ago during a camping trip in Pennsylvania. He does not remember developing a rash at that time. The patient has congenital hearing loss and wears a hearing aid. He takes no daily medications and has no known allergies. Temperature is 36.7 C (98 F) and blood pressure is 100/70 mm Hg. Physical examination shows a well-appearing child with a moderately swollen, warm, and mildly tender left knee. There is no erythema. Minimal pain is elicited with full extension of the knee. The patient is able to stand and bear weight. Sensation is intact. Capillary refill in the bilateral lower extremities is brisk. There are no rashes or petechiae. Laboratory results are as follows:
Complete blood count
Leukocytes
10,000/mm3
Neutrophils
70%
C-reactive protein
5 mg/L
Erythrocyte sedimentation rate
40 mm/hr
Arthrocentesis of the left knee is performed, and synovial fluid analysis reveals a white blood cell count of 18,000/mm³ with 85% neutrophils.
Item 1 of 2
Which of the following tests is most likely to identify the cause of this patient’s condition?
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 2
Left knee arthrocentesis relieves the patient’s swelling, and he is now able to walk almost normally. After 3 days, the patient returns for a follow-up visit. His parents are concerned about his ability to participate in sports. A mild effusion is present on left knee examination. Laboratory results are as follows:
Immunologic and rheumatologic studies
Anti-citrullinated peptide antibodies
pending
Antistreptolysin O titers
pending
Rheumatoid factor
15 U/mL (normal: <40)
Enzyme-linked immunosorbent assay for Lyme disease
pending
Western blot for Lyme disease
pending
Synovial fluid
Gram stain
negative
Bacterial culture
no growth
Which of the following is the most accurate description regarding this patient’s prognosis?
CorrectIncorrect -
Question 3 of 40
3. Question
A 6-year-old girl is brought to the office by her parents due to swelling on the right side of her neck. Two weeks ago, the patient’s mother first noticed a mass on her daughter’s neck; although the mass size remains unchanged, it has become more painful. Initially, her parents tried to treat the pain with ibuprofen and warm compresses, but with minimal relief. A 7-day course of oral clindamycin resulted in no improvement. The mass has become so painful that the patient is unable to fall asleep and tries not to turn her head. Today, she reports a foreign body sensation in her eyes and increased tearing. She has had increased fatigue and decreased appetite but no fever, weight loss, or difficulty swallowing. The patient has environmental allergies and seborrhea. She has a kitten and 2 hamsters. Temperature is 37.2 C (99 F). Examination of the right eye shows injected conjunctivae and scant clear discharge. The left eye is unaffected. Tympanic membranes are clear bilaterally. The posterior oropharynx is clear and without erythema or exudates. There is a 3-cm (1.2-in), tender, indurated, mobile cervical lymph node and a smaller 1-cm, tender, preauricular lymph node, both on the right side of the neck. Which of the following complications is most likely to develop in this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
A 17-year-old Caucasian boy is brought to the emergency department due to 3 days of worsening cough productive of green sputum. He has also had fever, fatigue, and chest pain with deep inspiration. For the past several years, the patient has had a cough on most days, but his current symptoms are worse than usual. He has had multiple hospitalizations for pneumonia, most recently 18 months ago. He also had a partial small bowel obstruction as a newborn. The patient takes several inhaled and oral medications daily. His sister has similar medical problems. Temperature is 102.3 F (39.1 C) and respirations are 22/min; oxygen saturation is 87% on room air. Examination shows a thin patient in moderate respiratory distress. Cardiac examination is normal. Auscultation of the lungs reveals crackles and scattered wheezes throughout, most prominent at the left base. Chest x-ray reveals hyperinflation, enlarged perihilar lymph nodes, and prominent bronchovascular markings. In addition to vancomycin, the most appropriate initial antimicrobial therapy for this patient should include which of the following?
CorrectIncorrect -
Question 5 of 40
5. Question
A 3-year-old girl is brought to the office for intermittent crampy abdominal pain that has been present for 4 months. Initially, the pain was associated with episodes of loose stool. Over the past month, the patient has had intermittent painful constipation. For the past 3 days, she has had flatus but not stooled. Her appetite has decreased and she has lost 1.5 kg (3.3 lb) since these episodes started. The patient has no significant medical history other than an episode of coughing and wheezing 6 months ago while she and her family were visiting relatives in Venezuela. Her immunizations are up to date, and she takes no medications. Temperature is 36.7 C (98 F), pulse is 108/min, and respirations are 20/min. On physical examination, the patient is awake but appears tired. The mucous membranes are moist. The lungs are clear to auscultation without wheezing or rales. The abdomen is distended and mildly tender, with no rebound or guarding; hyperactive bowel sounds are present. There is no hepatosplenomegaly. Laboratory evaluation reveals the following:
Complete blood count
Hemoglobin
12.6 g/dL
Platelets
240,000/mm³
Leukocytes
8,200/mm³
Neutrophils
48%
Eosinophils
20%
Lymphocytes
19%
Monocytes
3%
Liver function studies
Albumin
2.8 g/dL
Appropriate tests are performed, and the diagnosis is discussed with the family. Which of the following is the most accurate statement regarding this patient’s prognosis?
CorrectIncorrect -
Question 6 of 40
6. Question
A 2-month-old boy is brought to the office by his parents for well-child care. The infant was born at term via spontaneous vaginal delivery to a primigravid mother who developed acute hepatitis B infection during the third trimester. Both parents have a history of intravenous heroin use, and the father also has chronic, active hepatitis B. The parents entered a detoxification program after her diagnosis and no longer use illicit substances. The parents say, “We are terrified that he might develop hepatitis, too – it’s all we can think about.” The infant received hepatitis B immunoglobulin and vaccination at birth. The patient is gaining weight well and is formula feeding exclusively. Since his last visit, he has begun making cooing sounds and smiling. Vital signs are normal. Abdominal examination, including liver size, is unremarkable. The sclerae are white. The remainder of the physical examination is unremarkable. Which of the following is the most appropriate next step in this infant’s care?
CorrectIncorrect -
Question 7 of 40
7. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 17-year-old girl comes to the office for evaluation of a generalized rash. The rash was present when she woke up this morning and does not feel painful or itchy. For the past 10 days, the patient has had a sore throat, fever, fatigue, and body aches. She had a bottle of amoxicillin from a recent episode of pharyngitis and took a few pills this week, but the symptoms did not resolve. Her only medical problem was major depression, which resolved with behavioral therapy 3 years ago. She is sexually active and takes oral contraceptive pills. The patient takes no other medications. She does not use tobacco, alcohol, or illicit drugs. Temperature is 38 C (100.4 F), blood pressure is 110/76 mm Hg, pulse is 88/min, and respirations are 16/min. Physical examination demonstrates an awake but tired-appearing adolescent. There is no rhinorrhea, tympanic membranes are clear, and tonsils are enlarged and erythematous with white exudate bilaterally. There is tender cervical lymphadenopathy but no neck stiffness. S1 and S2 are normal. Lungs are clear to auscultation bilaterally. The abdomen is soft and nontender with mild hepatosplenomegaly. A diffuse, erythematous, blanching, maculopapular rash is seen on the chest, abdomen, and extremities. Laboratory results are as follows:
Complete blood count
Hemoglobin
12 g/dL
Hematocrit
34%
Platelets
240,000/mm3
Leukocytes
15,000/mm3
Liver function studies
Total bilirubin
1.3 mg/dL
Aspartate aminotransferase
87 U/L
Alanine aminotransferase
74 U/L
Item 1 of 2
In addition to discontinuing antibiotics, which of the following is the most appropriate management for this patient’s rash?
CorrectIncorrect -
Question 8 of 40
8. Question
Item 2 of 2
An appropriate diagnosis is made and the correct management is initiated. Which of the following is a true statement about the patient’s condition?
CorrectIncorrect -
Question 9 of 40
9. Question
An 8-year-old boy is brought to the physician for sore throat and fever that began yesterday. He has no rhinorrhea, congestion, cough, or facial pain but has been complaining of abdominal pain. He took acetaminophen with no relief of throat or abdominal pain. The boy’s past medical history is significant for 2 episodes of otitis media during infancy. He has no medication allergies. Physical examination shows enlarged tonsils with exudates and tender anterior cervical lymphadenopathy. The rapid antigen test for Streptococcus pyogenes is positive. Which of the following is the appropriate duration and rationale for treatment for this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
An 18-month-old boy is brought to the office for right ear pain. About 4 weeks ago, he had fever and right ear pain and was prescribed a 10-day course of high-dose amoxicillin for acute otitis media; he completed the course and had a normal follow-up visit 2 weeks ago. While on the medication, he experienced improvement in his symptoms. For the past 3 days, he has been tugging on his right ear and crying; he developed fever today. He has no nasal congestion, neck stiffness, cough, emesis, or other symptoms. He is otherwise healthy and takes no medications. His immunizations are up to date. Temperature is 38.5 C (101.3 F), blood pressure is 108/66 mm Hg, pulse is 96/min, and respirations are 21/min. Physical examination demonstrates an alert, uncomfortable child. Pupils are equal and reactive; the conjunctivae are injected bilaterally and have purulent discharge. There is no rhinorrhea or sinus tenderness. The external ears appear normal and are not painful to manipulation; there is no drainage in the external canal. The right tympanic membrane is erythematous, bulging, and immobile on pneumatic air insufflation. The left tympanic membrane appears normal. Both mastoids are nontender and nonerythematous. The neck is nontender and has full range of motion. Cardiopulmonary examination is normal.
Item 1 of 2
Which of the following is the most likely cause of this patient’s current symptoms?
CorrectIncorrect -
Question 11 of 40
11. Question
Item 2 of 2
An appropriate diagnosis is made, and the treatment options are discussed with the patient’s mother. What is the most appropriate next step in management of this boy’s condition?
CorrectIncorrect -
Question 12 of 40
12. Question
A 4-hour-old infant is evaluated in the neonatal intensive care unit. The infant was born at 37 weeks gestation via cesarean delivery to a healthy 33-year-old primigravid woman. Apgar scores were 6 and 8, at 1 and 5 minutes, respectively. The delivery was complicated by arrest of descent and nonreassuring fetal heart rate. The mother’s laboratory testing from the first prenatal visit demonstrated negative IgG titers to rubella but was otherwise normal. Fetal anatomy ultrasound at 20 weeks gestation showed no abnormalities. The mother traveled to South America at 15 weeks gestation for a family emergency and returned 2 weeks later. She smoked half a pack of cigarettes a day throughout the pregnancy but did not use alcohol or illicit drugs. She declined influenza and tetanus-diphtheria-acellular pertussis vaccines during pregnancy. The infant’s vital signs are normal. Height and weight are at the 20th percentile; head circumference is at the 95th percentile. Cardiac examination reveals a normal rate and regular rhythm. Abdominal examination reveals hepatomegaly but no other palpable masses. A head CT scan reveals hydrocephalus and diffuse intracranial calcifications. Which of the following best explains this infant’s examination findings?
CorrectIncorrect -
Question 13 of 40
13. Question
The following vignette applies to the next 2 items.
A 10-year-old girl is brought to the emergency department for evaluation of a bite wound. Last night, the girl had a fight with her 12-year-old stepbrother, who bit her on the forearm. This morning, the girl’s arm “looks worse.” The stepbrother is HIV-positive and acquired it from his mother at birth. He takes antiretroviral therapy; his most recent CD4 count was 1100 cells/µL, and his HIV viral load was undetectable. The patient has no known medical problems, and takes no medications. Her vital signs are normal. Examination shows 2 deep puncture wounds on the left forearm. There is warmth, erythema, and swelling around the bite marks. The skin is mildly tender to palpation. No fluctuance is palpated.
Item 1 of 2
The patient is at greatest risk for developing an infection from which of the following organisms?
CorrectIncorrect -
Question 14 of 40
14. Question
Item 2 of 2
The wound is irrigated thoroughly with saline and local wound care is provided. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 15-month-old girl is brought to the urgent care center due to 4 days of fever. Her father says, “Our entire family was sick with a cold last week, but no one had a fever for this long.” The patient’s symptoms began with rhinorrhea, cough, sore throat, and fever with daily temperatures >38.9 C (102 F). Three days ago, she developed bilateral conjunctival erythema with watery discharge. Yesterday, an erythematous rash appeared on her cheeks and slowly spread to the rest of her body. She attends day care 5 days a week, and several other children have been ill with similar symptoms, one of whom is currently hospitalized. The patient is otherwise healthy with no significant medical history. Her parents refused immunizations when she was age 12 months, as she had a fever after vaccination at age 6 months. Temperature is 39.4 C (103 F). Physical examination shows an ill-appearing girl lying in her father’s arms. A maculopapular rash is present on the face, trunk, and proximal extremities. Bilateral conjunctivae are erythematous without discharge, and there are multiple anterior cervical lymph nodes bilaterally that are 3-5 mm (0.12-0.2 in). The hands, feet, and oropharynx appear normal. Which of the following is the most likely cause of this patient’s symptoms?
CorrectIncorrect -
Question 16 of 40
16. Question
A 1-month-old girl is brought to the office by her parents due to worsening diaper rash. The parents first noticed red bumps in the diaper area a week ago. They tried changing the brand of diapers and wipes and have been applying baby powder. The rash has spread over the past 2 days and formed pustules that drain yellow fluid. This morning, the parents report that the patient felt warm; she has also been fussy and is refusing to feed or nap. She has neither vomited nor had diarrhea. The patient does not attend day care and has no sick contacts. Temperature is 38.5 C (101.3 F), pulse is 160/min, and respirations are 40/min. Oxygen saturation is 100% on room air. Examination reveals an irritable, crying infant. The anterior fontanelle is flat. The tympanic membranes are clear. Cardiopulmonary examination reveals no murmurs or abnormal lung sounds. The patient has crusted, erythematous papules and pustules scattered over the lower abdomen, diaper area, and upper thighs. The remainder of the examination is unremarkable. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 3-year-old girl is brought to the emergency department due to pain and fever. Two days ago, the patient developed mild abdominal and back pain. The fever began yesterday morning and reached 40.1 C (104.2 F) last night. Over the past 8 hours, she had 6 episodes of emesis but has since tolerated a few sips of water. The patient has a history of constipation since the start of toilet training at age 2 and has pellet-like stools once a week. She has frequent urinary accidents during the day and night. The patient takes no medications and has no other medical conditions. Vaccinations are up to date. Temperature is 40 C (104 F), blood pressure is 95/70 mm Hg, pulse is 110/min, and respirations are 20/min. Physical examination shows a tired-appearing girl with dry mucous membranes. She has right costovertebral tenderness. The abdomen is soft, nontender, and nondistended. The remainder of the examination is unremarkable. Laboratory results are as follows:
Complete blood count
Hemoglobin
13 g/dL
Platelets
260,000/mm3
Leukocytes
16,500/mm3
Urinalysis
Blood
negative
Glucose
negative
Ketones
positive
Leukocyte esterase
positive
Nitrites
positive
White blood cells
50/hpf
Red blood cells
9/hpf
Blood and urine culture results are pending. A 20-mL/kg normal saline bolus is administered. The patient has another episode of emesis and an additional void in the emergency department.
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 18 of 40
18. Question
Item 2 of 2
The patient is admitted to the hospital, and intravenous ceftriaxone is started. Urine culture is positive for Escherichia coli that is sensitive to third-generation cephalosporins. Blood culture is negative. After 48 hours, the patient is tolerating oral fluids and is afebrile. She is discharged from the hospital on oral cefdinir. Which of the following should be recommended to reduce the risk for infection recurrence in this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
A 16-year-old girl is brought to the emergency department with abdominal pain and diarrhea. The patient first noticed severe crampy abdominal pain 8 days ago after returning from a 3-day cruise in the Caribbean. Soon after, she developed watery diarrhea that has persisted and progressively worsened. The patient has had minimal oral intake due to nausea. Temperature is 39.2 C (102.6 F), blood pressure is 86/50 mm Hg, pulse is 128/min, and respirations are 20/min. The abdomen is distended and diffusely tender to palpation. Abdominal ultrasound reveals several distended bowel loops with thickened mucosal walls prominent along the entire colon and distal ileum. There is no visible free air, and the appendix appears normal. A stool culture is pending, but a rapid stool test is positive for enterotoxigenic Escherichia coli and negative for Shiga toxin. An intravenous fluid bolus is given with no change in vital signs. Which of the following is most appropriate in management of this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A previously healthy 5-year-old boy is brought to the physician with 2 days of sore throat. He has some pain with swallowing but is drinking fluids normally. He also has fever but no rhinorrhea, cough, or congestion. The boy has no known allergies and his immunizations are up-to-date. He recently started kindergarten, and other children at the school have been ill. His temperature is 38.9 C (102 F), blood pressure is 110/60 mm Hg, pulse is 98/min, and respirations are 20/min. Physical examination shows purulent exudates on the tonsils and posterior pharynx. Anterior cervical nodes are enlarged and tender. Lungs are clear to auscultation. A rapid streptococcal antigen test result is positive. What is the best next step in management of this patient?
CorrectIncorrect -
Question 21 of 40
21. Question
A 16-year-old boy is brought to an urgent care center by his father due to a rash. The rash started as a small, red area on his thigh about 5 days ago. The patient says, “I first noticed the rash the day after I went hiking. I got a lot of bug bites so I didn’t think much of it at first.” The area has since increased in size and is tender to the touch. The patient has had no fever or other rashes. He has no medical issues and is up to date on immunizations. He is on the school wrestling team and lives with his parents, grandparents, and 2 younger siblings. His grandfather was recently diagnosed with shingles; all other family members are healthy. Vital signs are normal. Physical examination reveals a well-appearing boy in no distress. Skin examination reveals a poorly demarcated, flat 8 cm x 8 cm area of tender, warm, confluent erythema on the anterior left thigh. There is no fluctuance or drainage. The remainder of the examination is unremarkable. Which of the following pathogens is the most likely cause of this patient’s rash?
CorrectIncorrect -
Question 22 of 40
22. Question
A 4-year-old girl is brought to the office due to a cat bite. Her parents say that the girl and her friend were attempting to dress up the family’s cat when it bit the patient on the right thumb. The bite occurred approximately an hour ago. The parents washed the girl’s thumb with soap and water before bringing her to the office. The cat has been with the family since it was a kitten and is fully vaccinated. The girl has a history of anaphylaxis following peanut and soy exposure, and her parents carry injectable epinephrine. Vital signs are within normal limits. The patient has minimal pain. Examination reveals a single puncture wound on the pad of the right thumb. There is no erythema, drainage, or tenderness to palpation. Range of motion is normal. The remainder of the examination is unremarkable. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 9-year-old boy is brought to the emergency department for fever and headache. He has had a runny nose, sore throat, and tactile temperatures for the last few days. The patient’s headache started 2 days ago and has progressively worsened despite taking acetaminophen every 4 hours. After he awoke this morning with vomiting, he appeared confused, which prompted this visit. Two weeks ago, his 4-year-old sister had a febrile illness with rash and mouth sores. The patient has no chronic medical conditions, and immunizations are up to date. Temperature is 39.5 C (103.1 F), blood pressure is 102/62 mm Hg, pulse is 122/min, and respirations are 24/min. He is drowsy but arousable. Pupils are equal and reactive to light, and funduscopic examination is normal. Cardiopulmonary examination is normal. The abdomen is soft and nontender. Bending the patient’s neck elicits flexion of his knees and hips. The tone on the right side of the body is increased, and the right arm is weak. Deep tendon reflexes are brisk on the right compared to the left. Which of the following is the best initial treatment for this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
A newborn boy is being evaluated in the nursery. He was born via normal spontaneous vaginal delivery with no complications. His mother did not receive prenatal care during pregnancy, and the estimated gestational age by her last menstrual period is 39 weeks. The infant has a weight of 2.4 kg (5 lb, 3 oz, 1st percentile), length of 46 cm (18 in, 2nd percentile), and head circumference of 32 cm (12.6 in, 2nd percentile). Physical examination shows a nondysmorphic, small for gestational age infant with several nonblanching, purpuric lesions over his trunk, face, and extremities. Red reflex is absent bilaterally. Cardiac examination reveals a continuous murmur that is loudest over the left infraclavicular region, and an enlarged spleen and liver are palpated in the abdomen. The patient fails the newborn hearing test bilaterally. Head ultrasound is normal. Which of the following is the most likely diagnosis for this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 10-week-old boy is brought to the office for a follow-up visit. As part of his routine immunization schedule, the patient received the first dose of the Haemophilus influenzae type b (Hib) conjugate vaccine when he was 8 weeks old. However, following vaccine administration, he developed anaphylaxis, requiring epinephrine administration and hospitalization. As a result, the decision was made not to administer additional doses of the Hib vaccine. The patient was born full-term by uncomplicated vaginal delivery and has otherwise been healthy. Physical examination is unremarkable. His older brother has completed the full vaccination course. This patient is at highest risk of which of the following infections compared to his brother?
CorrectIncorrect -
Question 26 of 40
26. Question
A healthy 12-month-old boy is brought to the physician for a routine examination. He started walking last week and can say “mama,” “dada,” “night-night,” and “go.” He eats a well-rounded diet and drinks whole milk twice a day. The patient lives with his mother, who is 17 weeks pregnant. His growth parameters and physical examination are normal. He is scheduled to receive measles-mumps-rubella, varicella, inactivated poliovirus, and pneumococcal conjugate vaccinations today. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
A 6-year-old girl is brought to a walk-in clinic for evaluation of growth. The patient and her family immigrated to the United States from Haiti 2 months ago. For the past 3 months, decreased appetite has led to the loss of several pounds. The patient has had occasional episodes of abdominal discomfort and diarrhea. The family denies any recent changes to her diet. There is no gross blood or mucus in the stool, and the patient has no fever. A mild cough early in the course of symptoms has since resolved. The patient received all age-appropriate vaccinations prior to immigration. She was also immunized in infancy for bacille Calmette-Guérin. Skin tuberculin testing at the time of immigration showed 2 mm induration. Temperature is 36.7 C (98.1 F), pulse is 102/min, and respirations are 18/min. Height is 120 cm (4 ft, 10th percentile) and weight is 19 kg (41.9 lb, <5th percentile). Physical examination shows a slightly distended abdomen with soft, hyperactive bowel sounds. There is generalized mild tenderness to deep palpation. No guarding, rebound tenderness, or hepatosplenomegaly is present. Fecal occult blood test is positive. Laboratory results are as follows:
Complete blood count
Hemoglobin
9.4 g/dL
Mean corpuscular volume
65 µm3
Platelets
380,000/mm3
Leukocytes
7,400/mm3
Neutrophils
65%
Eosinophils
15%
Lymphocytes
20%
Liver function tests
Albumin
2.5 g/dL
Aspartate aminotransferase (SGOT)
37 U/L
Alanine aminotransferase (SGPT)
24 U/L
Serum HIV antibody screen
negative
Which of the following diagnostic studies is most likely to be abnormal in this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 5-month-old boy is brought to the emergency department due to a diffuse rash. The patient has had a high fever, irritability, and decreased appetite for 4 days. Two days ago, he developed a rash that started with red spots on his face that has now spread across his body. The patient also developed a runny nose, a nonproductive cough, and red, watery eyes at fever onset. He has had no emesis or diarrhea. Temperature is 39.4 C (102.9 F), blood pressure is 100/70 mm Hg, pulse is 124/min, and respirations are 18/min. The patient is awake and alert but appears uncomfortable and irritable. The conjunctivae are injected bilaterally without discharge, and there is copious clear rhinorrhea. No oropharyngeal erythema or exudate is present, and the tympanic membranes are clear. The neck is supple without lymphadenopathy. Cardiopulmonary and abdominal examinations are unremarkable. There is an erythematous, morbilliform rash on the face, trunk, and extremities; some areas are confluent and nonblanching. Which of the following would be most helpful for preventing complications of this patient’s current condition?
CorrectIncorrect -
Question 29 of 40
29. Question
A 15-year-old boy is brought to the office due to fever. He has had fever, chills, fatigue, and myalgias for the past 10 days. He has lost some weight, which was attributed to poor appetite. Three weeks ago, the patient and his family returned from a trip to the Dominican Republic; he has not traveled anywhere else. There are no sick contacts at home. The patient has no significant medical history and takes no medications. Temperature is 38.3 C (101 F), blood pressure is 110/60 mm Hg, and pulse is 108/min. Physical examination shows a tired-looking boy in no acute distress. The tympanic membranes are not erythematous; mucous membranes are moist; and tonsils are enlarged and erythematous with white exudate. S1 and S2 are normal without murmurs. The lungs are clear to auscultation bilaterally. Lymphadenopathy is present in the anterior cervical, posterior cervical, axillary, and inguinal chains. The abdomen is soft and nontender. Laboratory results are as follows:
Complete blood count
Hemoglobin
14 g/dL
Hematocrit
38%
Platelets
200,000/mm3
Leukocytes
12,000/mm3
Segmented neutrophils
45%
Lymphocytes
49%
Monocytes
6%
The peripheral blood smear is shown in the image:
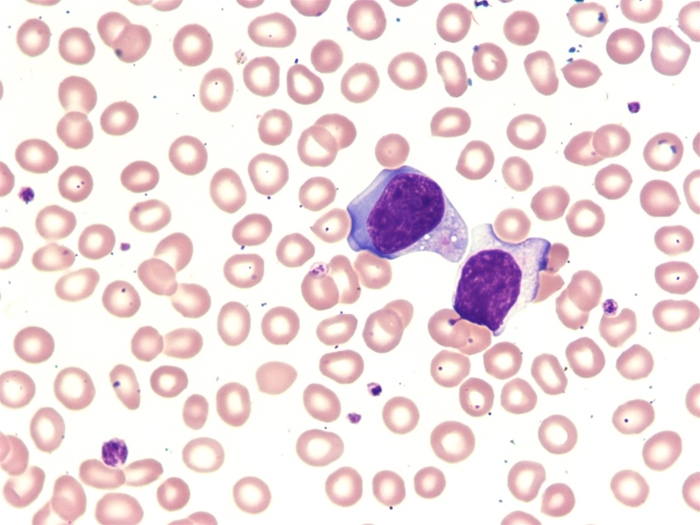
What is the most likely reason for these findings?
CorrectIncorrect -
Question 30 of 40
30. Question
An 8-year-old girl is brought to the office by her mother for evaluation of possible tuberculosis (TB). The patient’s younger brother was recently diagnosed with active pulmonary TB, which he contracted from their grandmother. The patient has been in close contact with her brother but has had no fever, night sweats, cough, anorexia, or weight loss. She had a negative TB skin test at the time of immigration from Southeast Asia 2 years ago. The patient has not received the bacille Calmette-Guérin vaccine but is up to date with other recommended vaccinations. Vital signs are within normal limits. No abnormalities are noted on physical examination. Interferon-gamma release assay is positive, and chest radiography is normal. Cultures of a gastric aspirate obtained from her younger brother show acid-fast bacilli that are resistant to isoniazid (INH) but sensitive to other anti-TB drugs. Which of the following is the most appropriate management for this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 6-month-old girl is brought to the office in January for well-child care. The patient is formula-feeding exclusively and has not yet started solid foods. She is voiding and stooling normally, and her growth and developmental milestones are appropriate for age. Today, she is due for the third dose of diphtheria-tetanus-pertussis, inactivated polio, Haemophilus influenzae type b, pneumococcal, and hepatitis B vaccines. The patient has not received an influenza vaccine, but she has received all previous immunizations with no adverse reactions. Her mother states, “I have several concerns about vaccinations. Is it safe to give my daughter shots if she had fever last week? The fever lasted only a day, but she is still coughing and congested. I also read that the flu shot contains egg, and I’m worried about an allergic reaction because my husband is allergic to eggs, and I don’t know how my daughter will react. Finally, I just found out that I’m pregnant, and I am afraid of exposure to germs from the vaccines.” Temperature is 36.7 C (98 F), pulse is 118/min, and respirations are 28/min. Physical examination shows nasal congestion, clear rhinorrhea, and clear postnasal drip. The lungs are clear to auscultation and the rest of the examination is normal. Which of the following is the most appropriate recommendation for this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 6-month-old girl is brought to the clinic by her mother for evaluation of fever and rash. Yesterday, the patient had a fever that resolved with antipyretics. This morning, she has been fussy and tired. The patient has had no cough, rhinorrhea, vomiting, or diarrhea. She attends day care, but the mother is not sure if other children have been ill. The patient was born at term and has no chronic medical conditions. Temperature is 38.1 C (100.6 F). Other vital signs are normal. Physical examination shows a mildly ill-appearing infant with several superficial ulcers scattered across the buccal mucosa and soft palate. Mucous membranes are moist, and the oropharynx is otherwise normal, without erythema, tonsillar enlargement, or exudates. Skin examination shows multiple macular, maculopapular, and vesicular lesions on the buttocks, palms, and soles; lesions are present in the interdigital spaces as well. There are no excoriations. The remainder of the examination is unremarkable. Which of the following is the most likely etiology of this patient’s examination findings?
CorrectIncorrect -
Question 33 of 40
33. Question
The following vignette applies to the next 2 items
A 16-year-old boy is brought to the emergency department via ambulance. The boy is accompanied by the school nurse, who notes that he has had a day of headache and generalized body aches that did not respond to acetaminophen. He felt well enough to attend school and to work his part-time job at a local hardware store after school for 2 hours yesterday. However, this morning his headache worsened and he was extremely drowsy. The paramedics administered intravenous normal saline; no other interventions were required during transport. As soon as he arrives in the emergency department, he becomes lethargic, has a seizure, and is immediately intubated by a resident physician. Subsequent evaluation reveals that the patient has acute meningococcal meningitis.
Item 1 of 2
In addition to the patient’s family members, which of the following contacts requires antibiotic prophylaxis to prevent the development of meningococcal meningitis?
CorrectIncorrect -
Question 34 of 40
34. Question
Item 2 of 2
The individuals requiring antibiotic prophylaxis are identified and contacted. Which of the following is the most appropriate therapy for chemoprophylaxis against meningococcal meningitis?
CorrectIncorrect -
Question 35 of 40
35. Question
A 3-year-old boy is brought to the emergency department due to 10 days of diarrhea. The diarrhea started out watery but has become bloody over the past few days although he is stooling less frequently. He has voided only twice in the past 24 hours. Temperature is 38.3 C (101 F), blood pressure is 96/62 mmHg, heart rate is 145/min. He is difficult to arouse and appears pale. He is tachycardic with otherwise unremarkable heart and lung sounds. His abdomen is soft, mildly distended, and tender to palpation in the left lower quadrant. There are no rashes. Initial laboratory studies show:
Complete blood count
Hemoglobin
7.2 g/dL
Platelets
60,000/mm3
Leukocytes
16,000/mm3
Neutrophils
70%
Eosinophils
3%
Lymphocytes
20%
Monocytes
10%
Serum chemistry
Blood urea nitrogen
50 mg/dL
Creatinine
1.2 mg/dL
Numerous fragmented red blood cells are noted on blood smear. Stool culture is pending, and PCR testing reveals Shigella dysenteriae type 1. Which of the following is the most appropriate therapy in this patient?
CorrectIncorrect -
Question 36 of 40
36. Question
A 2-year-old boy is brought to the office for follow-up. He was last seen 3 weeks ago for an episode of acute otitis media with symptoms of fever, crankiness, runny nose, and ear pain. Prior to this, he was healthy with no chronic medical conditions and with growth and developmental milestones appropriate for age. Examination at that time showed copious clear rhinorrhea and a bulging, erythematous right tympanic membrane. The patient was prescribed a 10-day course of amoxicillin. His mother reports that he has completed the course and his symptoms have improved: Fever has resolved, he no longer is cranky or indicates ear pain, and his appetite and activity level have returned to baseline. He has had occasional nasal congestion but no cough. Temperature is 36.7 C (98 F), pulse is 106/min, and respirations are 18/min. The patient is awake, alert, and in no acute distress. The head is normocephalic and atraumatic. The pupils are equal and reactive with normal fundi. The nares are patent with clear rhinorrhea; there is no erythema or exudate in the pharynx. The left tympanic membrane is normal; the right tympanic membrane is slightly retracted with yellow fluid behind the membrane and decreased mobility on pneumatic otoscopy. The neck is supple without lymphadenopathy. S1 and S2 are normal without murmurs. The lungs are clear to auscultation bilaterally. There are no rashes or skin lesions. What is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
The following vignette applies to the next 2 items.
An 8-year-old girl is brought to the physician for abnormal behavior. She has been acting inappropriately, crying, and laughing without apparent reason for the past 2 weeks. At school, she was restless and easily distracted. Last week, her parents noted strange movements of the girl’s hands that improved when she slept. On the day before presentation, her parents noticed rapid jerking movements of her face and feet. The girl has had minor, self-resolving upper respiratory infections but has otherwise been healthy. She takes no medications and her vaccinations are up-to-date. Examination shows an alert and cooperative girl with normal vital signs. Facial grimacing and tongue fasciculations are seen. The lungs are clear to auscultation and a II/VI holosystolic murmur is heard at the apex. When the girl speaks, distinct changes in the volume and pitch of her voice are noted. Muscular tone is mildly decreased globally. Pronator sign is positive, and the relaxation phase of the patellar reflex is delayed.
Item 1 of 2
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 38 of 40
38. Question
Item 2 of 2
The child’s diagnosis is discussed with her parents, who would like to know more about treatment of the condition. Which of the following is the most appropriate medication for this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 5-year-old boy is brought to the office during his summer vacation due to sore throat, fatigue, and mild headache of 2 days duration. The patient has pain with swallowing and has not eaten much in the past day but is drinking small amounts of fluids. He has no underlying health conditions, and review of systems is otherwise negative. The patient takes no medications and has no allergies. Temperature is 39 C (102.2 F). Examination shows pharyngeal erythema with vesicles on the posterior soft palate and no cervical lymphadenopathy. Cardiovascular, respiratory, and abdominal examinations are within normal limits. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 6-year-old boy is brought to the emergency department due to difficulty breathing. His mother states that he had a mild sore throat yesterday but seemed to respond to over-the-counter analgesics. She adds, “I noticed that my son felt warm, and his voice sounded raspy and hoarse. However, he was sleeping comfortably until an hour ago when he woke up suddenly with rapid, labored breathing.” The patient has no cough, runny nose, emesis, or diarrhea. He recently attended a family wedding where several guests were ill. Medical history is significant only for multiple episodes of otitis media and occasional upper respiratory infections. Other than analgesics for this illness, he takes no medications and has not been vaccinated. Temperature is 40 C (104 F), blood pressure is 105/70 mm Hg, pulse is 128/min, and respirations are 46/min. Examination shows an agitated-appearing boy who is leaning forward with his neck extended and mouth open wide. His tongue is protruding, and he is drooling heavily. There is mild inspiratory stridor with no wheezing or crackles, and subcostal and intercostal retractions are present. Heart sounds are normal without murmurs. There are no rashes or skin lesions. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect
