Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 54-year-old woman comes to the emergency department due to 12 hours of constant upper abdominal discomfort, nausea, and vomiting. The patient had a large dinner, went to bed feeling well, and was awakened by severe pain. In the past year, she has had brief similar episodes, but the pain was never this persistent. She has had no diarrhea or dysuria. Medical history includes gastroesophageal reflux, hyperlipidemia, and type 2 diabetes mellitus. The patient does not use alcohol, tobacco, or illicit drugs. Temperature is 38.3 C (100.9 F), blood pressure is 140/90 mm Hg, pulse is 110/min, and respirations are 20/min. BMI is 33.2 kg/m2. The lungs are clear to auscultation and heart sounds are normal. Abdominal examination reveals moderate tenderness in the right upper quadrant with voluntary guarding. There is no rebound tenderness. Laboratory results are as follows:
Complete blood count
Hemoglobin
13 mg/dL
Platelets
240,000/mm3
Leukocytes
16,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
4.2 mEq/L
Bicarbonate
24 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Liver function studies
Total bilirubin
0.3 mg/dL
Alkaline phosphatase
65 U/L
Aspartate aminotransferase (SGOT)
16 U/L
Alanine aminotransferase (SGPT)
22 U/L
Lipase
20 U/L
Ultrasound of the abdomen reveals several small gallstones without gallbladder wall edema or sonographic Murphy sign. The common bile duct is not enlarged. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 2 of 40
2. Question
The following vignette applies to the next 2 items
A 50-year-old man comes to the emergency department due to unremitting pain in his left buttock near the anus. He also has fever and malaise. Although he is uncertain when the discomfort first began, he notes that the pain has increased significantly over the past 24 hours and he has been unable to pass stool because of it. He has never experienced symptoms like this. Ten years ago, he was diagnosed with type 2 diabetes mellitus, and he currently takes insulin. Temperature is 38.7 C (101.7 F), blood pressure is 128/86 mm Hg, and pulse is 95/min. On digital rectal examination, sphincter tone is intact, but there is tenderness and fluctuance along the left rectal wall that are palpable 5 cm above the external sphincter. There is no crepitus in the perineum.
Item 1 of 2
What is the most appropriate next step in management of this patient?CorrectIncorrect -
Question 3 of 40
3. Question
Item 2 of 2
The patient is treated appropriately. To minimize risk for complications, he is advised to promptly schedule a follow-up visit with his primary care physician. Patients with anorectal abscesses are at greatest risk for which of the following conditions?CorrectIncorrect -
Question 4 of 40
4. Question
A 22-year-old male presents to the emergency department complaining of fever, abdominal pain, and vomiting. He has had these symptoms for the past four days, but has not sought medical attention because of concerns over the cost of treatment. On examination, the patient appears acutely ill. There is right lower quadrant tenderness with rebound as well as a palpable mass. CT scan of the abdomen and pelvis demonstrates a periappendiceal fluid collection. Culture of this fluid would most likely isolate which of the following organisms?
CorrectIncorrect -
Question 5 of 40
5. Question
The following vignette applies to the next 3 items
A 65-year-old man is brought to the emergency department by his wife due to severe upper-abdominal pain. The pain began suddenly 4 hours ago while he was watching television; it radiates to the back and is exacerbated by any movement. The patient has had gastroesophageal reflux disease for many years and has been taking over-the-counter antacids for symptom control. He also has hypertension, which is controlled with a thiazide diuretic. He walks 5 miles daily. The patient has been consuming large amounts of milk and other dairy products to relieve “burning” symptoms in his stomach. His temperature is 37.8 C (100 F), blood pressure is 110/62 mm Hg, pulse is 110/min, and respirations are 22/min. He lies flat and motionless on the bed. His mucous membranes are dry. Abdominal examination shows marked tenderness on superficial palpation. The patient does not allow any further palpation of the abdomen. Electrocardiogram shows sinus tachycardia.
Item 1 of 3
Which of the following is the best initial test for this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
Item 2 of 3
Further evaluation shows pneumoperitoneum on the upright chest x-ray. The patient’s white blood cell count is 11,300/μL, creatinine is 1.1 mg/dL, and lactic acid level is 2.1 mg/dL. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
Item 3 of 3
The patient was managed operatively, and he recovers well. Three years later, he comes to the emergency department with a 1-day history of nausea, vomiting, upper-abdominal pain, and distension. An abdominal radiograph reveals the presence of multiple air-fluid levels in the small intestine consistent with intestinal obstruction. Which of the following is the most likely mechanism of his intestinal obstruction?
CorrectIncorrect -
Question 8 of 40
8. Question
A 62 year-old Caucasian man is brought to the emergency department (ED) with complaints of nausea, vomiting, crampy lower abdominal pain and distension over the past two days. His last bowel movement was four days ago. His wife tells you that he has been unable to eat anything for the past 24 hours due to repeated episodes of vomiting. His past medical history includes hypertension, hyperlipidemia, and peptic ulcer disease. His current medications include thiazide diuretics, atorvastatin, and pantoprazole. He had an appendectomy at the age of 36 years, and surgical repair of a perforated peptic ulcer 8 years ago. His temperature is 36.7C (98F), blood pressure is 124/62 mmHg, respiratory rate is 22/min and heart rate is 96/min. His mucous membranes are dry. Abdominal examination reveals a distended abdomen with increased bowel sounds, a tympanic note throughout the abdomen, and tenderness on deep palpation over the lower abdomen. The rest of the examination is unremarkable. His initial blood work reveals marked electrolyte abnormalities. An obstruction series done in the ED reveals multiple air fluid levels in the small intestine consistent with a diagnosis of small bowel obstruction. There is some air seen in the distal colon. What is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 32-year-old Hispanic man comes to the emergency department after an episode of choking in the restaurant. He was drinking and dining with his friends at a local restaurant, when he accidentally choked on a fish bone. He initially felt a sharp painful sensation, but this subsided to a vague discomfort after drinking four glasses of water. He denies having any difficulty in breathing, and only has a slight difficulty in swallowing his saliva. He has a mild discomfort and can still feel the fish bone lodged in the back of his throat. On a quick examination of his upper oropharynx, you do not see any evidence of fishbone. Which of the following is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
A 40-year-old man comes to the office due to gastrointestinal symptoms. He has a 2-month history of abdominal bloating, excessive flatulence, and watery stools that occur both during the day and at night. The patient had similar symptoms a year ago but had marked improvement following a 10-day course of amoxicillin-clavulanic acid for sinusitis. Medical history is notable for obesity, for which he underwent a Roux-en-Y gastric bypass procedure 5 years ago. The patient takes multiple vitamin supplements as recommended following surgery and does not use tobacco or alcohol. Blood pressure is 112/70 mm Hg. BMI is 27 kg/m2. The abdomen is soft and nontender; bowel sounds are normal. Rectal examination shows no abnormalities. Complete blood count and comprehensive metabolic panel are normal. Stool is negative for leukocytes and occult blood. HIV testing is negative. Serum TSH is normal. Which of the following is the most likely cause of this patient’s recurrent symptoms?
CorrectIncorrect -
Question 11 of 40
11. Question
A 55-year-old man comes to the emergency department due to a 3-day history of abdominal cramps and diarrhea. He has had 5-7 watery stools a day, including at night. Three weeks ago, the patient was hospitalized for a perforated peptic ulcer that was complicated by peritonitis; he received antibiotics and underwent abdominal washout and distal gastrectomy. The initial postoperative course was uncomplicated. Temperature is 38.3 C (100.9 F), blood pressure is 116/74 mm Hg, and pulse is 96/min. Abdominal examination shows mild distension and diffuse tenderness. Bowel sounds are normal. The surgical wounds are clean, intact, and without discharge. Which of the following is the most likely cause of this patient’s diarrhea?
CorrectIncorrect -
Question 12 of 40
12. Question
A 63-year-old man comes to the emergency department due to worsening pain in the right upper quadrant, nausea, and vomiting since last night. He woke up at midnight with abdominal discomfort and nausea. He could not fall back to sleep due to the increasing pain as well as malaise and shaking chills. The patient had 2 episodes of vomiting this morning. He has gastroesophageal reflux disease and takes esomeprazole occasionally. He also has a history of hypertension and osteoarthritis. The patient drinks a glass of wine daily with dinner but does not use tobacco or illicit drugs. On initial evaluation, he appears uncomfortable due to pain. Temperature is 38.3 C (101 F), blood pressure is 96/65 mm Hg, pulse is 102/min and regular, and respirations are 18/min. Physical examination shows mild scleral icterus. Mucous membranes are dry. The abdomen is soft and nondistended, with moderate tenderness in the right upper quadrant. There is no rebound tenderness. Bowel sounds are active. Laboratory results are as follows:
Complete blood count
Hemoglobin
13 g/dL
Leukocytes
16,000/mm3
Liver function studies
Total bilirubin
3.3 mg/dL
Direct bilirubin
2.5 mg/dL
Alkaline phosphatase
470 U/L
Aspartate aminotransferase
62 U/L
Alanine aminotransferase
74 U/L
Serum creatinine is 0.9 mg/dL. Abdominal ultrasonography reveals increased liver echotexture consistent with fatty infiltration, several small gallstones, and dilated biliary ducts. Intravenous fluids and empiric antibiotics are administered, and the blood pressure and tachycardia improve. Which of the following is the best management strategy for this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
A 62-year-old woman comes to the office due to a sense of heaviness and discomfort in her right groin. Her discomfort is worse with standing and coughing, and is relieved by lying flat. She also noticed a painful bulging mass at the same site 2 days ago, which resolved spontaneously after 2 hours. She has a history of breast cancer and chronic bronchitis. She had a left mastectomy at age 48 and 2 cesarean sections at age 28 and 33. She smokes a pack of cigarettes daily. On examination and Valsalva maneuver, a right-sided femoral hernia that is easily reducible is found. There is no evidence of incarceration or strangulation. Which of the following is the most appropriate next step?
CorrectIncorrect -
Question 14 of 40
14. Question
A 76-year-old man is brought from the nursing home to the emergency department for evaluation of rectal discomfort that has worsened over the past 3 days. The patient also had an episode of a small amount of rectal bleeding. His other medical problems include chronic constipation, benign prostatic hypertrophy, and chronic obstructive pulmonary disease. His temperature is 37.2 C (99 F), blood pressure is 110/60 mm Hg, pulse is 100/min, and respirations are 20/min. Examination of the anal area shows a thick, protruding, rectal mucosal mass with bluish discoloration, concentric rings, and friability. He appears to be in moderate distress due to rectal discomfort. Which of the following is the most appropriate next step in the management of this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 43-year-old woman comes to the emergency department due to midepigastric abdominal pain. The pain is sharp, radiates to her back, and is accompanied by nausea, vomiting, and malaise. Her symptoms started approximately 24 hours earlier. For the past 6 months she has had intermittent, colicky abdominal pain that occurs after meals. The patient’s medical problems include hypertension, depression, and recurrent urinary tract infections. Medications include lisinopril, amlodipine, and fluoxetine. She has no known drug allergies and does not use tobacco, alcohol, or illicit drugs. Family history is notable for ovarian cancer in her mother. Temperature is 37.1 C (98.8 F), blood pressure is 146/92 mm Hg, pulse is 85/min, and respirations are 14/min. Physical examination reveals moist mucous membranes, no lymphadenopathy, clear lung fields, and normal S1 and S2. The abdomen is soft and tender in the midepigastrium without rigidity or rebound tenderness. Bowel sounds are normoactive. The remainder of the examination is normal. Laboratory results are as follows:
Complete blood count
Leukocytes
9,000/mm3
Hemoglobin
14.4 g/dL
Platelets
280,000/mm3
Serum chemistry
Sodium
136 mEq/L
Potassium
3.3 mEq/L
Chloride
98 mEq/L
Bicarbonate
28 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Calcium
9.6 mg/dL
Glucose
88 mg/dL
Liver function studies
Total protein
7.8 g/dL
Albumin
4.3 g/dL
Total bilirubin
1.3 mg/dL
Alkaline phosphatase
220 U/L
Aspartate aminotransferase (SGOT)
101 U/L
Alanine aminotransferase (SGPT)
122 U/L
Lipase
752 U/L (normal: 0-160)
The patient is hospitalized and treated with supportive care. Abdominal ultrasound reveals multiple gallstones that are 3-5 mm in diameter, but no abnormalities are seen in the common bile duct. Lipid panel shows triglycerides of 150 mg/dL. On the third day of hospitalization, the patient is symptom-free, she tolerates oral feeding, and liver enzymes have normalized. Which of the following treatment options is most appropriate to prevent further episodes of pancreatitis?
CorrectIncorrect -
Question 16 of 40
16. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 44-year-old man with a medical history of food allergy to peanuts is brought to the emergency department for an allergic reaction. The patient developed the acute onset of dyspnea and wheezing shortly after ingesting a cookie. His symptoms progressed to difficulty swallowing and swelling of the face and tongue. On arrival, temperature is 36.9 C (98.4 F), pulse is 115/min, blood pressure is 85/74 mm Hg, and respirations are 28/min. Oxygen saturation is 93% on a nonrebreather face mask. He is anxious and pale with swollen lips, swollen tongue, and inspiratory stridor. On lung auscultation, bilateral wheezing is present. Intramuscular epinephrine, intravenous fluids, and racemic epinephrine via nebulizer are administered without improvement. The patient’s distress is increasing, and he is becoming more agitated. The decision to intubate using awake fiberoptic nasotracheal intubation is made.
Item 1 of 2
Which of the following medications would be the best choice to aid in awake fiberoptic nasotracheal intubation in this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
Item 2 of 2
Severe swelling of the upper airway is seen on laryngoscopy, and 3 attempts to pass the endotracheal tube are unsuccessful. The patient’s blood pressure is 70/40 mm Hg, pulse is 75/min, and respirations are 40/min. Oxygen saturation is 72% on a nonrebreather face mask. What is the best next step in management of this patient?
CorrectIncorrect -
Question 18 of 40
18. Question
A 23-year-old man is brought to the emergency department after a head-on motor vehicle collision in which both vehicles were traveling at moderate speed. The patient was a restrained driver in the collision. He has no significant medical history and takes no medications. Initially he reports pelvic pain only. Blood pressure on arrival is 132/65 mm Hg and pulse is 102/min. He is given bolus intravenous fluids and opioid analgesics for pain. The patient’s cervical spine is clinically cleared for acute fractures, and he is diagnosed by plain film with a pelvic fracture. A pelvic binder is applied. One hour after initial presentation, the patient is short of breath and has chest pain. Blood pressure is 122/70 mm Hg and pulse is 84/min. Pulse oximetry shows 95% on room air. Physical examination shows the patient to be in no apparent distress lying supine. Mucous membranes are moist. No jugular venous distension or tracheal deviation is present. The patient is not using accessory respiratory muscles, and no penetrating chest trauma is noted. Breath sounds are diminished on the right upper lung field with hyperresonance to percussion and absent fremitus. The abdomen is soft and nontender. No distension, hepatomegaly, splenomegaly, or free fluid is present. The remainder of the examination is normal. Which of the following is the best initial test to assess for the suspected diagnosis of pneumothorax in this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A previously healthy 40-year-old man is evaluated in the burn intensive care unit for decreasing urine output. He had no medical history until 3 days ago when he was involved in a motor vehicle collision and car fire. The patient suffered severe burns to >60% of his body as well as multiple long bone fractures, but no internal injuries to his chest or abdomen. He has been receiving intravenous fluids and wound care. Urine output was initially 0.5 mL/kg/hr but has decreased significantly over the last 8 hours, despite additional crystalloid boluses. Temperature is 37 C (98.5 F), blood pressure is 88/65 mm Hg, and pulse is 125/min. Oxygen saturation is 92% on 40% FiO2. The patient is intubated, sedated, and mechanically ventilated. Burn dressings are present on his abdomen, back, and all 4 extremities. Jugular venous distension is present. Mild basilar crackles are present with normal inspiratory and expiratory air movement. Heart sounds are normal. The abdomen is distended and tense. A urinary catheter is draining a small amount of yellow urine. Bilateral lower extremities have 3+ pitting edema. During the examination, the peak pressure alarm on the ventilator sounds multiple times. Chest x-ray reveals low lung volumes with elevated hemidiaphragms. The patient’s routine laboratory results from 2 hours earlier include the following:
Complete blood count
Hemoglobin
8 g/dL
Hematocrit
24%
Serum chemistry
Blood urea nitrogen
38 mg/dL
Creatinine
2.2 mg/dL
Item 1 of 2
Which of the following is the most likely primary cause of this patient’s current condition?
CorrectIncorrect -
Question 20 of 40
20. Question
Item 2 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 21 of 40
21. Question
A 72-year-old man is evaluated in his hospital room for hypoxemia and shortness of breath. He says, “I just can’t seem to get enough air to breathe.” He also has a cough that is intermittently productive of white sputum. The patient underwent emergency open colectomy 3 days ago for cecal volvulus. His course was complicated by postoperative respiratory failure, and he remained on a mechanical ventilator for 48 hours. He was extubated 12 hours ago and has since had significant pain around the incision site, receiving opioid medications as needed. Medical history includes hypertension, ischemic stroke with resulting left-sided weakness, and coronary artery disease. The patient has smoked a pack of cigarettes a day for the last 45 years. He has no history of alcohol or drug abuse. Temperature is 37 C (98.6 F), blood pressure is 145/90 mm Hg, pulse is 90/min, and respirations are 24/min. Oxygen saturation is 87% on room air. The patient appears chronically ill and drowsy. Examination shows moist mucous membranes and normal jugular venous pressure. Respirations are shallow and limited by pain around the incision. The patient has a weak cough with no stridor. Breath sounds are diminished at the bilateral lung bases, with scattered rhonchi. Heart sounds are normal. The abdomen is mildly distended and tender near the incision site. The surgical wound appears clean and is without discharge. There is 1+ bilateral edema of the lower extremities. A complete blood count and metabolic panel are normal. Arterial blood gas analysis on room air shows a pH of 7.47, PaO2 of 56 mm Hg, and PaCO2 of 33 mm Hg. Chest x-ray reveals small lung volumes and bilateral linear densities of the lower lobe. In addition to the supplemental oxygen to correct the hypoxemia, which of the following is most beneficial for treating this patient’s respiratory symptoms?
CorrectIncorrect -
Question 22 of 40
22. Question
A 62-year-old woman comes to the office for a preoperative evaluation 3 days before undergoing elective cholecystectomy. Over the past few months, she has had transient episodes of postprandial abdominal pain after large meals. Abdominal ultrasound confirms multiple gallstones. The patient feels well overall but has had 3 days of cough productive of green sputum and worsened dyspnea. She has a history of chronic obstructive pulmonary disease, myocardial infarction with stenting of the right coronary artery, hypertension, and obesity. She currently takes aspirin, lisinopril, rosuvastatin, amlodipine, albuterol, and ipratropium. She has had no previous surgeries. The patient has smoked a pack of cigarettes daily for 35 years but does not use alcohol or illicit drugs. Vital signs are within normal limits. Physical examination reveals moist mucous membranes and normal jugular venous pressure. Pulmonary auscultation indicates wheezing over the bilateral lung fields and prolonged expiration. There are no heart murmurs. No edema is present, and the remainder of the examination is normal. Which of the following interventions is most likely to reduce the incidence of postoperative pulmonary complications in this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
The following vignette applies to the next 2 items.
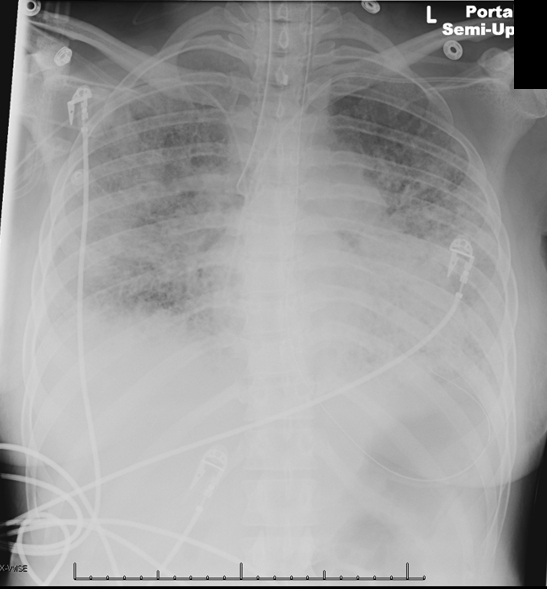
A 72-year-old woman is found to be severely short of breath at her skilled nursing facility. The patient was recently hospitalized for vertebral osteomyelitis and discharged 2 weeks ago to complete a 6-week course of piperacillin-tazobactam via a peripherally inserted central venous catheter. Her dyspnea began only with exertion but is now also present at rest. Medical history includes coronary artery disease with ischemic cardiomyopathy, chronic obstructive pulmonary disease, and chronic kidney disease. She has had 2 hospitalizations for heart failure over the last year; noninvasive positive-pressure ventilation was required. Paramedics observe the patient to be obtunded with agonal respirations and rales throughout the bilateral lung fields. Oxygen saturation is 72% on room air. She is intubated and transferred to the emergency department. On arrival, the patient is minimally responsive to stimuli. Temperature is 36.7 C (98 F), blood pressure is 115/65 mm Hg, and pulse is 110/min and regular. The patient’s oxygen saturation is 88% on 100% inspired oxygen. BMI is 19 kg/m2. The trachea is midline. On physical examination, rales are heard on the right side and markedly decreased breath sounds on the left side of the chest. S3 is heard. There is 2+ bilateral peripheral edema. A chest x-ray reveals the following:
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
Item 2 of 2
After the intervention is performed, the patient’s oxygenation improves. She is transferred to the medical intensive care unit and treated with diuretics and bronchodilators. Two days later, her ventilation requirements have improved to 50% inspired oxygen and 5 cm of positive end-expiratory pressure. The patient’s respirations suddenly become dys-synchronous with the ventilator, and her oxygen saturation drops to 85%. Tidal volume spontaneously decreases from 350 to 200 mL. Temperature is 37.2 C (99 F), blood pressure is 125/60 mm Hg, pulse is 110/min, and respirations are 25/min. Physical examination shows that the trachea is midline and the endotracheal tube is in place. No jugular venous distension is present. Breath sounds are markedly decreased on the right side. A portable chest x-ray reveals the following:

Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 60-year-old man is taken to the post-anesthesia care unit less than an hour after an elective laparoscopic cholecystectomy. The surgery was uneventful and the patient was extubated in the recovery room. Medical history is significant for hypertension, hyperlipidemia, chronic kidney disease, and obstructive sleep apnea. The patient has no history of alcohol, tobacco, or recreational drug use. Temperature is 100 F (37.8 C), blood pressure is 125/65 mm Hg, pulse is 75/min, and respirations are 7/min. Oxygen saturation is 100% on 4 L of oxygen via nasal cannula. When the nurse attempts to wean the patient from the oxygen, pulse oximetry drops to 87%. The patient is somnolent but arousable when his name is called. Auscultation reveals shallow respirations with no rales, wheezing, or rhonchi. Abdominal examination shows a surgical wound with mild distension and tympany. There is no lower extremity edema. Chest x-ray reveals mild hypoinflation. Arterial blood gas analysis on 36% FiO2 is as follows:
pH
7.25
PaO2
170 mm Hg
PaCO2
58 mm Hg
Which of the following is the most likely cause of this patient’s requirement of supplemental oxygen?
CorrectIncorrect -
Question 26 of 40
26. Question
A 36-year-old factory worker is brought to the emergency department after a fire at the chemical plant where he worked. The patient was trapped for several minutes by the fire and had to be rescued by firefighters. He has pain in his face, neck, and arms. The patient has no pertinent medical history. Temperature is 37.2 C (99 F), blood pressure is 140/80 mm Hg, pulse is 130/min, and respirations are 20/min. Pulse oximetry is 100% on a nonrebreather mask. He is awake, alert, and oriented. There are some superficial partial-thickness burns to the patient’s face and anterior neck. His hair and beard are singed. The patient’s voice is normal, the lungs are clear, and no stridor is present. There are deep partial- and full-thickness burns involving the anterior surface of his bilateral upper extremities. Pulses are normal. Carboxyhemoglobin level is 15%. Intravenous fluids and opioids are administered. What is the best next step in management of this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
A 17-year-old girl is admitted to a level 1 trauma center due to severe head trauma during a motor vehicle collision. CT scan of the head reveals cerebral contusion, edema, and intraventricular hemorrhage. Aggressive medical interventions, including decompressive craniectomy, are performed, but she remains comatose after 2 weeks of intensive care. She is mechanically ventilated and breathes above the set ventilator rate. Five days ago, she developed ventilator-associated pneumonia associated with sepsis and acute kidney injury. Her oxygenation has now improved, her hemodynamic status is stable without vasopressor use, and her renal function has begun to recover. A neurologist determines that the patient has suffered a “catastrophic” neurologic event and is not expected to have significant neurologic recovery. The patient’s family wants to honor her prior wishes to be an organ donor. Which of the following best applies to this patient at this time?
CorrectIncorrect -
Question 28 of 40
28. Question
A 32-year-old man comes to the office for evaluation of gradually decreasing libido and intermittent inability to achieve erections for the past year. In addition, he has noticed decreased growth of facial hair. The patient is physically active, walking 60 minutes 4 or 5 times a week. He has a history of generalized anxiety disorder and has been taking sertraline for 3 years; he currently has no symptoms of depression or anxiety. The patient does not use tobacco, alcohol, or recreational drugs. Family history is unremarkable. Vital signs are normal. Height is 177 cm (5 ft 10 in). BMI is 24 kg/m2. The testes are small, soft, and descended bilaterally. No testicular mass is palpable. Physical examination is otherwise unremarkable. Laboratory results show a normal TSH level and comprehensive metabolic panel, but early morning serum testosterone, LH, and FSH are low. What is the best next step in management of this patient’s erectile dysfunction?
CorrectIncorrect -
Question 29 of 40
29. Question
A 16-year-old boy is brought to the emergency department due to severe scrotal pain. The patient had an abrupt onset of scrotal pain 6 hours ago. He tried to treat it with ibuprofen and ice packs, but it continued to worsen. The pain is now severe, making walking difficult. The patient is nauseated and vomited once but has had no fever or abdominal or flank pain. He has had no chronic medical conditions or previous surgeries. The patient attends high school, where he is the captain of the varsity soccer team and has daily afternoon practice. He is sexually active with 2 current partners and uses condoms only intermittently; he last had intercourse a week ago. The patient does not use tobacco, alcohol, or illicit drugs. Temperature is 37.2 C (99 F), blood pressure is 118/72 mm Hg, and pulse is 102/min. The abdomen is soft, nontender, and has no rebound or organomegaly. Bowel sounds are active. Genital examination reveals an exquisitely tender and swollen right testicle approximately 7 cm in its longest axis. Elevation of the testis exacerbates the pain. Which of the following is the most likely additional finding in this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 30-year-old man is in the recovery room following elective circumcision. There is no family history of bleeding disorders. The procedure was performed under sedation and local anesthesia without intraoperative complications. However, shortly after arrival at the recovery room, bleeding was noted at the surgical site, and a compressive elastic dressing was applied to the glans and distal shaft of the penis. Temperature is 36.7 C (98.1 F), blood pressure is 136/82 mm Hg, pulse is 92/min, and respirations are 14/min. The patient is alert and appears comfortable. The penile dressing is intact, with no evidence of residual bleeding. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
A 14-year-old boy is brought to the emergency department for evaluation of severe scrotal pain. Half an hour ago, the patient was accidentally hit in the scrotum during wrestling practice. He applied ice and took acetaminophen, neither of which relieved the pain. He has not tried urinating due to fear of the pain. The patient underwent a right orchiopexy as an infant due to unilateral cryptorchidism but has no chronic medical conditions. Temperature is 36.7 C (98.1 F), blood pressure is 114/76 mm Hg, and pulse is 108/min. Abdominal examination is unremarkable. There is moderate bruising on the right hemiscrotum but not on the medial thigh or perineum. The right testis is exquisitely tender to palpation but has normal contours. Bilateral testes retract with stroking of the medial thigh. The penis has no blood at the meatus or open wounds. Intravenous morphine provides significant pain relief, and the patient is able to urinate spontaneously. Urinalysis results are as follows:
Specific gravity
1.025
Blood
Negative
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
A 63-year-old man comes to the office for the evaluation of urinary urgency, hesitancy, nocturia, and a weak urinary stream. These symptoms have progressively worsened over the past year, despite being on doxazosin. He has not had any fever, abdominal pain, hematuria, malaise, or weight loss. He does not use tobacco or alcohol. Rectal examination reveals a smooth, firm enlargement of the prostate without any induration or asymmetry. Neurological examination is normal. His prostate-specific antigen level is elevated, and the option of transurethral resection of the prostate (TURP) is discussed. He is concerned about the complications of the procedure. Which of the following is the most likely expected complication of this procedure?
CorrectIncorrect -
Question 33 of 40
33. Question
A 9-month-old boy is brought to the office for follow-up of an undescended testis. Developmentally, the patient sits without support, babbles, and can pick up objects with his pointer finger and thumb. He is fed formula and eats table foods 3 times a day. He was born at 38 weeks gestation without complications during pregnancy or delivery. The patient takes no medications and has no allergies. He is up to date with vaccinations. Length, weight, and head circumference are at the 50th percentile. On physical examination, the infant is nondysmorphic, alert, and active and is crawling on the floor. The abdomen is soft, nontender, and nondistended. Genital examination shows absent rugae on the left hemiscrotum with a palpable testicle in the left inguinal canal; the right testicle is palpable in the right hemiscrotum. The penis appears normal with a centrally located urethral meatus, and the urinary stream is normal. The anus is patent with no lesions. Which of the following statements regarding this patient’s genitourinary condition is most accurate?
CorrectIncorrect -
Question 34 of 40
34. Question
A couple who is expecting a first child comes to the office to discuss circumcision. They recently learned that the baby is a boy, but they have not decided whether to have him circumcised. The father says that he is circumcised and had expected his son would also be. However, the mother says one of her closest friends thinks circumcision is “barbaric.” The couple wants to know the health implications of neonatal circumcision. Which of the following is the most appropriate response?
CorrectIncorrect -
Question 35 of 40
35. Question
A 65-year-old man with persistent atrial fibrillation comes to the emergency department due to a cold right foot. He has been inconsistent with anticoagulation therapy. Medical history also includes type 2 diabetes mellitus, hypertension, and chronic kidney disease with low-grade proteinuria. Blood pressure is 122/70 mm Hg and pulse is 112/min and irregular. On physical examination, the right leg is cold and dorsalis pedis and posterior tibial pulses are absent. An emergency angiogram reveals right popliteal artery occlusion. Thrombus aspiration is performed with good results. Two hours later, the patient has intense pain in his right leg accompanied by burning and “ants crawling” sensations. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 36 of 40
36. Question
A 62-year-old man is brought to the emergency department with severe pain and numbness in the right leg. The patient says, “I was watching television 2 hours ago when the pain started, and then my leg became numb.” Medical history includes coronary artery disease with a previous anterior wall myocardial infarction, heart failure with reduced ejection fraction, hypertension, and hyperlipidemia. He does not adhere regularly to prescribed medications. The patient does not smoke cigarettes but consumes alcohol occasionally. He appears to be in significant discomfort due to pain. Temperature is 36.7 C (98.1 F), blood pressure is 150/90 mm Hg, pulse is 102/min and regular, and respirations are 14/min. Physical examination shows a cool right lower extremity with delayed capillary refill. There is decreased sensation, but motor function is preserved. On Doppler examination, no pulses are detected at the right popliteal and dorsalis pedis arteries. Intravenous heparin infusion is initiated. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
A 24-year-old Caucasian male was involved in a major motor vehicle accident. The ambulance service that arrived several minutes after the accident found him dead. He was found in the driver’s seat, and the steering wheel in front of him was broken. Which of the following is the most likely cause of his death?
CorrectIncorrect -
Question 38 of 40
38. Question
A 68-year-old man is hospitalized after coronary artery bypass grafting surgery. The patient has a history of coronary artery disease treated with stenting of the right coronary artery several years ago. Medical history also includes hypertension, type 2 diabetes mellitus, and hypercholesterolemia. Over the past 6 months, the patient has had worsening angina, and cardiac catheterization revealed 80% stenosis of the left main artery and restenosis of the right coronary artery. Echocardiography showed a left ventricular ejection fraction of 40% with no valvular abnormalities. A 2-vessel coronary artery bypass grafting with a left internal mammary to the left anterior descending artery and a saphenous vein graft to the right coronary artery was performed. The intraoperative course was uncomplicated, and the patient was extubated 24 hours later. On the third postoperative day, the patient developed atrial fibrillation. He is hemodynamically stable with adequate urine output and good control of the postoperative pain. Serum electrolytes are within normal limits. The patient becomes concerned about the postoperative arrhythmia. Which of the following is the most accurate statement about this patient’s atrial fibrillation?
CorrectIncorrect -
Question 39 of 40
39. Question
A 68-year-old man comes to the emergency department due to 12 hours of worsening abdominal pain, nausea, and vomiting. The patient has had intermittent abdominal discomfort and nausea over the past several months but not to this severity. He has had no diarrhea, and his most recent bowel movement was 1 day ago. The patient has no known medical conditions and takes no medications. He has smoked a pack of cigarettes daily for 30 years and drinks 1 or 2 alcoholic beverages daily. Temperature is 38.5 C (101.3 F), blood pressure is 106/64 mm Hg, pulse is 112/min, and respirations are 18/min. On physical examination, the patient appears to be in discomfort and is diaphoretic. The abdomen is tender and rigid throughout. Bowel sounds are absent. Abdominal imaging shows free air under the diaphragm. Intravenous fluids and empiric antibiotics are started, and surgical consultation is obtained. While being prepared for laparotomy, the patient develops new-onset atrial fibrillation with a ventricular rate of 126/min. The patient reports no palpitations, chest pain, or dyspnea. Blood pressure is 116/70 mm Hg. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 58-year-old woman comes to the physician for a preoperative evaluation 2 weeks prior to an elective left knee replacement for severe osteoarthritis. Her other medical problems include hypertension, type 2 diabetes, hyperlipidemia, chronic obstructive pulmonary disease, osteoporosis, and gastroesophageal reflux disease. Her medications include amlodipine, atorvastatin, calcium carbonate, metformin, metoprolol, raloxifene, ramipril, pantoprazole, and daily salmeterol and ipratropium bromide metered-dose inhalers. She has no known drug allergies. She does not use tobacco, alcohol, or illicit drugs. Family history is not significant. Her blood pressure is 144/86 mm Hg, pulse is 62/min, and respirations are 12/min. Her BMI is 29 kg/m2. Physical examination shows left knee crepitus. Her serum creatinine level is 1.0 mg/dL. Which of the following medications should be discontinued now in preparation for the surgery?
CorrectIncorrect
