Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 2 items.
A 38-year-old man is brought to the emergency department due to sudden-onset shortness of breath and diaphoresis. He has no fever, chills, cough, or abdominal pain. The patient has no other medical problems and takes no medications. He had surgery for bilateral inguinal hernias at age 16. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 95/60 mm Hg, pulse is 116/min and regular, and respirations are 28/min. He is in marked respiratory distress. Pallor and diaphoresis are noted. His skin is velvety and has many atrophic scars. The apical impulse is hyperdynamic. Cardiac auscultation reveals a soft, early-systolic decrescendo murmur at the cardiac apex. S1 is barely audible; S2 is normal. Lung examination reveals bibasilar crackles. Jugular venous distension is present. The abdomen is soft, nontender, and nondistended. Neurologic examination shows no abnormalities. ECG shows sinus tachycardia with occasional premature ventricular complexes. Chest x-ray reveals no cardiomegaly, but bilateral alveolar infiltrates and hilar prominence are present.
Item 1 of 2
Which of the following is the most likely cause of this patient’s condition?
CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 2
The patient feels better after receiving appropriate therapy. A more detailed physical examination shows the presence of thoracolumbar scoliosis. Serial cardiac enzymes are negative. Arterial blood gas analysis shows respiratory alkalosis. Complete blood cell count and serum chemistry results are unremarkable. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 3 of 40
3. Question
A 62-year-old man comes to the office to establish care. He recently moved to the area and states that his physician was treating him for high blood pressure. The patient has no symptoms and feels healthy. He describes his lifestyle as mostly sedentary but reports no limitations with walking at a fast pace. Current medications are chlorthalidone and losartan. The patient has never smoked and does not drink alcohol. His father had open-heart surgery at age 70, but the patient cannot provide details. Blood pressure is 138/90 mm Hg and pulse is 72/min. An ejection-type systolic murmur is heard at the right upper sternal border consistent with aortic stenosis. Which of the following additional findings would be most suggestive of severe valvular dysfunction?
CorrectIncorrect -
Question 4 of 40
4. Question
A 55-year-old woman comes to the office due to exertional dyspnea for 3 months. The patient has had no chest pain. Medical history is significant for hypertension and chronic kidney disease. Medications include furosemide, amlodipine, and lisinopril. The patient has never smoked cigarettes. Temperature is 37 C (98.6 F), blood pressure is 128/80 mm Hg, and pulse is 80/min. Oxygen saturation is 98% on room air. BMI is 27 kg/m2. There is no jugular venous distension. Cardiopulmonary examination is normal. Trace bilateral pedal edema is present. Laboratory studies are as follow:
Hemoglobin
10.8 g/dL
Blood urea nitrogen
38 mg/dL
Serum creatinine
2.2 mg/dL
Estimated glomerular filtration rate
28 mL/min/1.73 m2
ECG is unremarkable. Chest x-ray reveals clear lung fields. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 5 of 40
5. Question
A 6-year-old boy is brought to the office by his mother for an annual physical examination. He has had no recent illnesses but has had intermittent pain in his legs during his soccer games for the past 3 months. The patient had no trauma preceding the onset of leg pain, has no numbness or tingling, and is able to walk without a limp. He was born at 38 weeks gestation via a spontaneous vaginal delivery with no complications. The patient has met all developmental milestones, and all of his immunizations are up to date. His father was recently diagnosed with hypertension at age 55, but there is no other significant family history. Temperature is 36.1 C (97 F), blood pressure is 135/88 mm Hg in the right upper extremity, pulse is 110/min, respirations are 24/min, and pulse oximetry is 98% on room air. Weight and height are at the 25th and 50th percentiles, respectively, for age. Physical examination shows a well-appearing boy who has no dysmorphic features and who smiles and fully cooperates. The lungs are clear to auscultation. Heart rhythm is normal. A 2/6 continuous murmur is heard over the left interscapular area. The lower extremities have no swelling, erythema, or tenderness. Further evaluation would most likely show which of the following findings?
CorrectIncorrect -
Question 6 of 40
6. Question
A 53-year-old woman comes to the emergency department after coughing up blood while at work. She has had no prior episodes but gives a lengthy history of shortness of breath, fatigue, palpitations, and cough while lying down. She has not seen a physician in many years. Her blood pressure is 122/70 mm Hg, pulse is 98/min, and respirations are 23/min. Her body mass index is 20 kg/m2. The patient appears anxious and fatigued. Jugular venous pressure is estimated at 9 cm H2O. Cardiac examination shows normal apical impulse with loud 1st heart sound and short apical low-pitched diastolic rumbling murmur. Bilateral crackles are heard. Electrocardiogram shows a broad-notched P wave in lead II as well as right axis deviation. Chest radiograph shows pulmonary edema, prominent pulmonary arteries at the hilum, elevation of the left mainstem bronchus, and left atrial enlargement with a flattening of the left heart border. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 7 of 40
7. Question
A 46-year-old woman comes to the emergency department due to progressive dyspnea over the last 2 days. The patient’s exercise tolerance has decreased dramatically and she had to sleep in a sitting position last night. She has no history of cardiovascular disease. The patient does not use tobacco or alcohol. Family history is unremarkable. Blood pressure is 110/65 mm Hg and pulse is 105/min and regular. The apical impulse is hyperdynamic. Cardiac auscultation reveals a diminished S1 and an apical holosystolic murmur radiating to the axilla. Diffuse pulmonary crackles are heard bilaterally. There is no peripheral edema. ECG shows sinus tachycardia but is otherwise unremarkable. Which of the following would most likely increase the ratio of forward flow volume to regurgitant flow volume in this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
A 43-year-old man comes to the physician for a follow-up visit. He was diagnosed with coronary artery disease and received a stent to the left circumflex artery a year ago. At that time, he was started on aspirin, clopidogrel, metoprolol, and atorvastatin. About a week ago, the patient was seen in the emergency department for pain in both thighs following a 15-mile walk sponsored by a local organization. His serum creatine kinase level was 500 units/L (normal 25-90 units/L). Atorvastatin was discontinued, and he was discharged with a prescription for ibuprofen. The patient also was advised to consult his primary care physician. His symptoms have improved markedly since discharge from the emergency department. His physical examination is normal. The patient’s most current lipid profile, performed about 15 days ago while on medication, shows low-density lipoprotein cholesterol of 132 mg/dL, triglycerides of 100 mg/dL, and high-density lipoprotein cholesterol of 40 mg/dL. He asks about restarting atorvastatin. Which of the following is the best recommendation for this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 48-year-old woman experiences increasing exertional dyspnea and exercise intolerance. The patient has a history of mitral valve prolapse with mitral regurgitation. She has no other medical conditions. Echocardiography demonstrates a myxomatous mitral valve with bileaflet prolapse, severe mitral regurgitation, and a left ventricular ejection fraction of 65%. After discussion of the risks and benefits of surgery, the patient undergoes surgical mitral valve replacement with a bileaflet mechanical valve. She has no intraoperative complications and has an uneventful postoperative course. Three months later, the patient reports no symptoms and has improvement in exercise tolerance. She is taking warfarin to prevent prosthetic valve thrombosis after the procedure. Which of the following is the best antithrombotic recommendation for this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
A 25-year-old man is brought to the emergency department after a syncopal episode that occurred during a powerlifting competition. The patient suddenly collapsed after he straightened from lowering the barbell from over his head to the floor. He was unconscious for approximately a minute. The patient reported feeling light-headed prior to collapsing but states that he frequently feels this way after standing or rising during competitive powerlifting matches. He reports no similar symptoms at other times. The patient has no known medical conditions. Family history is significant for hypertension. Temperature is 36.7 C (98.1 F), blood pressure is 110/60 mm Hg, pulse is 72/min, and respirations are 16/min. The patient is awake, alert, and oriented with normal speech. Dry mucous membranes are noted on oropharyngeal examination. Heart and lung examinations are normal. Strength is 5/5 in the upper and lower extremities, and gait is normal. ECG is normal. Laboratory results are as follows:
Complete blood count
Hemoglobin
18.2 g/dL
Hematocrit
54%
Platelets
380,000/mm3
Leukocytes
9,000/mm3
Serum chemistry
Sodium
140 mEq/L
Potassium
3.0 mEq/L
Chloride
104 mEq/L
Bicarbonate
24 mEq/L
Blood urea nitrogen
30 mg/dL
Creatinine
1.5 mg/dL
What is the best next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
A 55-year-old man comes to the emergency department due to palpitations that began earlier this morning. He was having tea when he suddenly started to experience fluttering in his chest. He tried walking around and taking deep breaths, but the feeling did not subside. The patient has previously felt his “‘heart skipping a beat” but has never had sustained palpitations as he did today. He has no lightheadedness, blurry vision, muscle weakness, chest pain, or shortness of breath. The patient has hypertension that is well controlled with valsartan and amlodipine. He does not use tobacco, alcohol, or recreational drugs. He has no medication allergies. His father had a stroke at age 65 and his mother has heart failure. On initial evaluation, the patient appears anxious and in mild discomfort due to palpitations. Blood pressure is 140/80 mm Hg and respirations are 19/min. Jugular venous pressure is estimated at 2 cm H2O above the sternal angle. Cardiac auscultation reveals no murmurs. Lungs are clear to auscultation. The abdomen is soft, nontender, and nondistended. Neurologic examination shows no abnormalities. The patient is placed on a telemetry monitor, and the ECG rhythm is shown in the exhibit. What is the most appropriate next step in management of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 12 of 40
12. Question
A 42-year-old woman comes to the clinic for a routine physical examination. She has no specific concerns, but on review of systems acknowledges that she has recently been getting tired easily. The patient also informs the physician of occasional palpitations, which she describes as a “fast heartbeat.” Family history is significant for hypertension and type 2 diabetes mellitus. She is a lifetime nonsmoker. The patient does not drink alcohol or use illicit drugs. Vital signs are normal. She was told in the past that she has “a heart problem” that she thinks is mitral valve prolapse. The patient was advised to follow-up with a cardiologist, but she says she had been feeling well and did not see a doctor. Which of the following physical findings would be most consistent with this diagnosis?
CorrectIncorrect -
Question 13 of 40
13. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
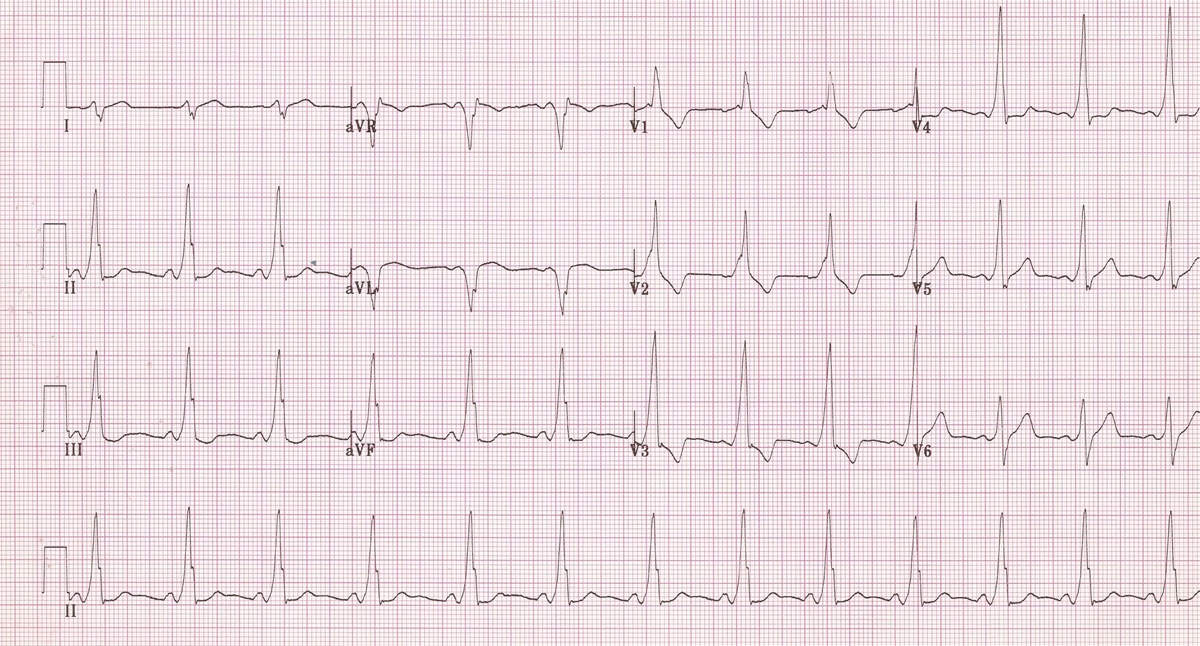
A 36-year-old man comes to the emergency department due to loss of consciousness. He was standing in a crowded subway station when he felt lightheaded, had a pounding sensation in his chest, and passed out. On awakening, he felt short of breath for a little while and then was “completely fine.” He has had no similar episodes, nor chest pain, confusion, tongue biting, or urinary incontinence. The night before, he was at a party with friends and consumed alcohol. Later he was nauseated and had 3 episodes of vomiting and one episode of diarrhea. In the emergency department, blood pressure is 124/68 mm Hg and pulse is 80/min. There is a small laceration above his right eyebrow. Cardiac examination shows normal heart sounds with regular rhythm. The lungs are clear to auscultation. Neurologic examination shows no abnormalities. ECG is shown in the exhibit.
Item 1 of 2
Which of the following is the most likely cause of this patient’s syncope?
CorrectIncorrect -
Question 14 of 40
14. Question
Item 2 of 2
The patient is hospitalized for observation. His serum electrolytes are within normal limits. Echocardiogram shows normal left ventricular size and function and no significant valvular abnormalities. During the hospital stay, he has another episode of lightheadedness when the telemetry revealed brief supraventricular tachycardia that resolved spontaneously. Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 15 of 40
15. Question
A 60-year-old man comes to the office for follow-up due to persistent atrial fibrillation. He reports occasional palpitations and poor exercise tolerance. For the past year, the patient’s atrial fibrillation has been managed with a rate-control strategy using metoprolol. Three months ago, his metoprolol dosage was increased for improved rate control, but today in the office, he reports that he was unable to tolerate the new dosage due to dizziness. Blood pressure is 110/70 mm Hg and pulse is 105/min and irregular. Examination shows no abnormalities. Echocardiography reveals left atrial enlargement, an ejection fraction of 59%, and no significant valvular disease. The patient is advised to remain on his previously tolerated metoprolol dose, and digoxin is added to the medication regimen. Four weeks later, he reports symptom improvement. Resting pulse is 84/min and irregular. Which of the following best explains digoxin’s effect on heart rate in this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
A 76-year-old man comes to the office due to leg discomfort. He describes intermittent swelling and heaviness in both legs over the past year. Medical history is significant for hypertension, hyperlipidemia, benign prostatic hyperplasia, and degenerative joint disease of both knees. The patient is retired and frequently volunteers as a hospital greeter. Vital signs are within normal limits. Estimated jugular venous pressure is normal. Cardiopulmonary examination reveals normal lung and heart sounds. The left lower extremity is shown in the exhibit; there are similar findings in the right lower extremity. Peripheral pulses are full and symmetric. Results of recent laboratory studies, including complete blood count, complete metabolic panel, and urine electrolytes, were within normal limits. Which of the following is the most appropriate next step in management of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 17 of 40
17. Question
A 67-year-old man has recurrent witnessed episodes of loss of consciousness while shaving. The episodes are characterized by a feeling of faintness followed by loss of consciousness, and each episode resolves after less than a minute. Blood pressure is 130/80 mm Hg and pulse is 80/min and regular; there are no significant changes in blood pressure or heart rate with supine and standing positions. Cardiac auscultation is normal with no murmurs or extra sounds. There are no neck bruits and the lungs are clear to auscultation. Which of the following factors is most likely contributing to this patient’s symptomatic episodes?
CorrectIncorrect -
Question 18 of 40
18. Question
An 82-year-old woman comes to the emergency department due to chest pain. The pain began when the patient was vacuuming and “felt as if someone placed my chest in a vise.” The pain improved after resting for 30 minutes, but she called her daughter, who brought her to the hospital. The pain began again while she was walking into the waiting room. The patient also reports mild nausea, weakness, and lightheadedness. She has a history of hypertension, for which she takes losartan, and a prior upper gastrointestinal bleed for which she underwent treatment for Helicobacter pylori. She has hyperlipidemia but did not tolerate simvastatin in the past due to muscle aches. The patient is a nonsmoker. She drinks a glass of wine on social occasions. She has a younger brother who recently underwent coronary artery bypass graft surgery. Blood pressure is 152/92 mm Hg, pulse is 92/min, and oxygen saturation is 96% on room air. The patient appears mildly uncomfortable. Examination reveals jugular venous distension and diffuse lung crackles. On cardiac auscultation, a low-pitched extra heart sound just after S2 is appreciated at the apex. The abdomen is soft and there is trace lower extremity edema bilaterally. ECG shows ST-segment depression in leads I, aVL, and V3-V6. Which of the following medications should be avoided in this patient at this time?
CorrectIncorrect -
Question 19 of 40
19. Question
A 58-year-old man with a 15-year history of hypertension comes to the emergency department after sudden-onset severe back pain. Temperature is 36.7 C (98.1 F), blood pressure is 180/105 mm Hg, pulse is 84/min, and respirations are 18/min. Funduscopic examination shows arteriolar wall thickening and occasional cotton-wool spots. The rest of the examination is within normal limits. Initial laboratory studies are normal except for serum blood urea nitrogen of 28 mg/dL and serum creatinine of 2.3 mg/dL. Transesophageal echocardiography reveals a dissection in the descending aorta. The patient is admitted to the coronary care unit and prescribed intravenous labetalol and nitroprusside infusion. After 2 days, he becomes agitated and confused and has an episode of vomiting. Blood pressure is 130/60 mm Hg, pulse is 50/min, and respirations are 10/min. During examination, the patient has a generalized tonic-clonic seizure. The results of a basic metabolic panel obtained just prior to the seizure are as follows:
Serum chemistry
Sodium
140 mEq/L
Potassium
4.8 mEq/L
Chloride
106 mEq/L
Bicarbonate
14 mEq/L
Blood urea nitrogen
30 mg/dL
Creatinine
2.4 mg/dL
Glucose
140 mg/dL
Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
A 32-year-old man is evaluated for a murmur, which was found during a preventive examination. He has no symptoms, and his past medical history is insignificant. The patient smokes a pack of cigarettes per day. He has no family history of cardiovascular disease or sudden death. Blood pressure is 132/80 mm Hg and heart rate is 68/min. The patient’s height is 178 cm. Body mass index is 31 kg/m2. A 2/6 ejection-type murmur is heard at the right upper sternal border. His physical examination is otherwise unremarkable. Transthoracic echocardiogram shows normal left atrial and left ventricular size, left ventricular ejection fraction of 60%, bicuspid aortic valve, and trivial aortic regurgitation. There is no evidence of aortic stenosis on Doppler echocardiography. For which of the following conditions should this patient be evaluated specifically?
CorrectIncorrect -
Question 21 of 40
21. Question
A 44-year-old man comes to the office for evaluation of a cardiac murmur. He was recently seen at an urgent care facility for a sinus infection and a murmur was discovered, for which follow-up was recommended. The patient has no cardiopulmonary symptoms and reports no prior health issues. He jogs or bikes several miles on most days of the week. He does not use tobacco, alcohol, or recreational drugs. Blood pressure is 120/70 mm Hg and pulse is 68/min and regular. Jugular venous pressure is normal. The point of maximal impulse is nondisplaced. S1 and S2 are normal with no gallop. There is a 3/6 systolic murmur best heard at the apex following an early systolic click. Transthoracic echocardiography reveals a dilated left atrium and left ventricle. The mitral valve leaflets are diffusely thickened from myxomatous degeneration. There is systolic prolapse of the posterior leaflet with eccentric mitral regurgitation. The regurgitant fraction is >50%, and the left ventricular ejection fraction is 55%. Which of the following is the strongest indication for mitral valve surgery in this patient?
CorrectIncorrect -
Question 22 of 40
22. Question
A 76-year-old man is admitted to the hospital with nausea, vomiting, and generalized abdominal distension. He has a long-standing history of type 2 diabetes mellitus. His medical follow-up has been poor. Physical examination and diagnostic workup are consistent with a complicated small-bowel obstruction. He undergoes exploratory laparotomy with no operative complications and is extubated postoperatively in the surgical intensive care unit. A few hours after extubation, the patient experiences sudden onset of chest discomfort, nausea, and marked diaphoresis. Temperature is 36.1 C (97 F), blood pressure is 84/50 mm Hg, pulse is 32/min, and respirations are 26/min. Examination shows minimal crackles at both bases. There are no murmurs on cardiac examination. Fingerstick glucose level is 150 mg/dL. ECG shows sinus bradycardia with 3-mm ST-segment elevations in leads II, III, and aVF. Immediate chest x-ray shows increased interstitial markings bilaterally. Intravenous normal saline infusion is started and intravenous atropine is administered without significant improvement. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 23 of 40
23. Question
A 32-year-old man is evaluated for syncope. The patient passed out once briefly when playing basketball and experienced no post-syncopal symptoms. Over the last year, he has tired easily and becomes short of breath when climbing 3–4 flights of stairs. The patient takes lansoprazole for acid reflux. In the past, a physician had told him that his blood pressure is “borderline.” The patient smokes half a pack of cigarettes a day. His paternal uncle died suddenly at age 30. Blood pressure is 152/90 mm Hg and pulse is 90/min. A 2/6 midsystolic murmur is heard at the left sternal border and accentuates on standing. Lungs are clear to auscultation. Echocardiography shows left atrial enlargement, interventricular septal thickness of 2 cm (normal <1.1 cm), and posterior left ventricular wall thickness of 0.9 cm (normal <1.1 cm). Left ventricular ejection fraction is 75%. There is systolic anterior motion of the mitral valve. At rest, peak instantaneous left ventricular outflow gradient is 30 mm Hg and increases to 45 mm Hg with Valsalva. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
A 65-year-old man comes to the office for evaluation of dyspnea with exertion for the past several months. He has had no chest pain, orthopnea, or paroxysmal nocturnal dyspnea. Medical history includes hypertension and heart failure with reduced ejection fraction. Recent echocardiography showed left ventricular ejection fraction of 40%. Coronary angiography performed 3 years ago revealed nonobstructive coronary artery disease. The patient takes sacubitril-valsartan, metoprolol, dapagliflozin, aspirin, and rosuvastatin. He smoked for 40 years and quit a year ago. Temperature is 37 C (98.6 F), blood pressure is 118/68 mm Hg, pulse is 72/min, and respirations are 18/min. BMI is 27 kg/m2. Jugular venous pressure is normal. On lung examination, breath sounds are decreased bilaterally with prolonged expiration. There is no peripheral edema. Chest x-ray shows mild cardiomegaly but is otherwise unremarkable. ECG demonstrates normal sinus rhythm with nonspecific T-wave changes, unchanged from 3 months ago. Laboratory studies reveal a serum creatinine level of 0.8 mg/dL, potassium of 4.1 mEq/L, and brain natriuretic peptide of 500 pg/mL (normal: <100 pg/mL). Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 25 of 40
25. Question
An 82-year-old man comes to the office for an annual follow-up visit. The patient says, “Over the last 2 months I have had several episodes of shortness of breath and dizziness while walking up the stairs. I also don’t have energy like I did before and feel fatigued even after a short stroll around the house.” The symptoms improve spontaneously after several minutes of rest. The patient has had no chest pain, cough, palpitations, or leg swelling. He sleeps flat on his back and does not wake up at night with shortness of breath. Medical history is significant for hypertension, hyperlipidemia, osteoarthritis, and diet-controlled type 2 diabetes mellitus. He is independent in his activities of daily living. He is a former smoker, with a 15-pack-year history, and quit over 20 years ago. Temperature is 37 C (98.6 F), blood pressure is 146/84 mm Hg, pulse is 78/min, and respirations are 14/min. BMI is 27.6 kg/m2. Pulse oximetry shows 98% while resting and breathing ambient air. Mucous membranes are moist. There is no jugular venous distension or lower extremity edema. Bilateral breath sounds are normal with no wheezing or crackles. Cardiac examination reveals that the point of maximal impulse is slightly displaced to the left and that there is an S4 gallop with no murmurs. Abdominal examination is unremarkable. The patient has mild crepitus of the knee joints with no effusion or tenderness. Basic laboratory studies are unremarkable. ECG shows sinus rhythm, evidence of left ventricular hypertrophy, and nonspecific ST-segment and T-wave changes. Different studies are being considered as part of the evaluation. Which of the following is likely to be most helpful in determining the cause of this patient’s symptoms?
CorrectIncorrect -
Question 26 of 40
26. Question
A 50-year-old man is brought to the emergency department due to chest pain and lightheadedness for the past hour. He was clearing away snow when he suddenly felt substernal chest pressure accompanied by cold sweats. The pain has been constant, radiates to the left jaw, and is not relieved by rest or the nitroglycerin spray he received in the ambulance. The patient has a history of well-controlled hypertension. He smokes occasionally, especially on weekends, but does not use alcohol. His father had a myocardial infarction at age 60. On examination, the patient appears to be in mild distress. The extremities are cold. Temperature is 36.1 C (97 F), blood pressure is 84/52 mm Hg, pulse is 34/min, and respirations are 16/min. Oxygen saturation is 94% on 4 L/min nasal cannula oxygen. Lung auscultation reveals crackles at both lung bases. There are no heart murmurs. The abdomen is soft and nontender. ECG shows sinus bradycardia with a 3-mm ST-segment elevation in leads II, III, and AVF. Which of the following is most appropriate as part of initial management for this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
A 62-year-old man with hypertension and heart failure comes to the office for follow-up 2 weeks after hospital discharge for acute decompensated heart failure. The patient becomes short of breath after walking 1 block or climbing a flight of stairs but does not have orthopnea, cough, or hemoptysis. Current medications include metoprolol succinate, sacubitril-valsartan, furosemide, and spironolactone. Blood pressure is 128/76 mm Hg and pulse is 80/min. Oxygen saturation is 95% on room air. Jugular venous pressure is estimated at 8 cm H2O. Lungs are clear to auscultation, and an S3 is heard at the apex. There is trace peripheral edema. Echocardiography shows left ventricular ejection fraction of 30%, mild mitral regurgitation, and mild pulmonary hypertension. The patient’s serum creatinine is 1.2 mg/dL, and serum potassium is 5.0 mEq/L. Which of the following is the best additional therapy for this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 70-year-old man is brought to the emergency department by his wife after he passed out earlier this morning. The patient was sitting in a chair watching TV when he lost consciousness for approximately 3 minutes before spontaneously recovering. He did not fall off the chair, and his wife did not observe any convulsive limb movements. There was no soiling of his clothes by urine or stool. She says, “Doc, it has never happened to him before. He was completely unresponsive and looked pale. I got really scared.” In the emergency department the patient has no headache, nausea, chest discomfort, or shortness of breath. He has no recollection of what happened and did not feel anything out of the ordinary beforehand. Medical history includes hypertension, hyperlipidemia, type 2 diabetes mellitus, and coronary artery disease. The patient had an anterolateral myocardial infarction 2 years ago and underwent coronary stent placement. Since then, he has had no episodes of angina. His lifestyle is sedentary and he spends little time outdoors. He becomes short of breath when climbing a flight of stairs. On initial evaluation the patient appears comfortable and asks if he can go home. Temperature is 36.7 C (98 F), blood pressure is 130/86 mm Hg sitting and 125/85 mm Hg standing, pulse is 78/min, and respirations are 16/min. Pulse oximetry shows 98% on room air. Neurologic examination is nonfocal. ECG shows normal sinus rhythm with anterolateral Q waves, unchanged from prior ECG. Blood cell counts, serum chemistry studies, and chest x-ray are within normal limits. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
A 68-year-old woman is referred for preoperative evaluation prior to breast implant removal. The patient was diagnosed with breast cancer 10 years ago and underwent left mastectomy, chemotherapy, and breast reconstruction. She has implant capsular contracture and wants the implant removed. The patient has no fatigue, chest pain, shortness of breath, or lightheadedness. She does not exercise but says she usually takes the stairs to her second-story office. Medical history is significant for nonischemic cardiomyopathy with reduced ejection fraction since completing chemotherapy. Echocardiogram 6 months ago showed an ejection fraction of 40% and mild mitral regurgitation. Other medical conditions include hypertension and dyslipidemia. She has a 20-pack-year history but quit smoking 10 years ago. Blood pressure is 134/78 mm Hg and pulse is 65/min. Physical examination shows no jugular venous distension. There is a 1/6 holosystolic murmur at the apex. The lungs are clear to auscultation and no peripheral edema is present. Preoperative laboratory studies are significant for a creatinine of 1.3 mg/dL. ECG shows sinus rhythm and nonspecific T-wave changes. Which of the following is the best preoperative management for this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 33-year-old woman comes to the office due to dyspnea on exertion for the past 15 months. The patient becomes breathless after walking a block at a slow pace and must also stop for breath halfway up a flight of stairs. A year ago, she could walk 10-12 blocks without limitations. The patient also becomes “light-headed” when stooping down to tie her shoes. She has no chest pain, palpitations, cough, or hemoptysis. Two years ago, the patient’s routine physical showed no abnormalities. She does not use tobacco, alcohol, or recreational drugs. Her mother has a history of breast cancer and “blood clots,” and her father had a stroke. The patient takes no prescription or over-the-counter medications. She has no known drug allergies. On examination, the patient appears comfortable at rest. Temperature is 36.7 C (98.1 F), blood pressure is 133/81 mm Hg, pulse is 84/min, and respirations are 16/min. Pulse oximetry shows 94% saturation on room air. BMI is 32 kg/m2. Cardiac auscultation demonstrates a prominent S2 loudest at the left second intercostal space and a grade 2/6 holosystolic murmur at the lower sternal border that increases with inspiration. The lungs are clear. There is no peripheral edema. Chest-x ray reveals prominent pulmonary arteries but no infiltrates. Office spirometry is normal. ECG shows normal sinus rhythm with right axis deviation.
Item 1 of 2
Which of the following is the most appropriate next step in management of this patient?CorrectIncorrect -
Question 31 of 40
31. Question
Item 2 of 2
Echocardiography demonstrates increased pulmonary artery systolic pressure, right ventricular dilation, and normal left ventricular size and function. Right-sided heart catheterization reveals a mean pulmonary artery pressure of 40 mm Hg (normal: ≤20) and a pulmonary capillary wedge pressure of 10 mm Hg. Further studies, including autoimmune serologies, pulmonary function tests, ventilation/perfusion scan, and polysomnography, are unremarkable. Treatment of this patient’s condition should include an inhibitor of which of the following targets?CorrectIncorrect -
Question 32 of 40
32. Question
A 45-year-old woman comes to the office for hypertension follow-up. She has been taking low-dose amlodipine for the past 2 years, and it has been effective in controlling her blood pressure without adverse effects. The patient has no other medical conditions. In the past year, she initiated and maintained an intensive diet and exercise program, resulting in a weight loss of 15 kg (33 lb). Since then, the patient’s blood pressure at home has been consistently 115-120/70-75 mm Hg. Office blood pressure today is 118/74 mm Hg. The patient says “I have worked really hard for the past year to lose weight, and I don’t like to take pills. Can I stop taking the blood pressure medication after this visit?” Which of the following is the best response to address the patient’s request?
CorrectIncorrect -
Question 33 of 40
33. Question
A 49-year-old woman comes to the emergency department with a 2-day history of fever, dysuria, and flank pain. The patient has a history of poorly controlled type 2 diabetes mellitus. Temperature is 38.3 C (101 F), blood pressure is 80/44 mm Hg, pulse is 134/min, and respirations are 34/min. On physical examination, the patient appears lethargic, flushed, and diaphoretic. Neck veins are flat. The lungs are clear on auscultation and heart sounds are normal. There is right-sided costovertebral tenderness. Which of the following hemodynamic parameters are most likely to be present in this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 34 of 40
34. Question
A 22-year-old woman is brought to the office by her mother because “she has been passing out.” The patient’s first episode occurred about a year ago when she split up with her boyfriend. A more recent episode was also provoked by strong emotion. Both episodes were preceded by nausea, light-headedness, weakness, and blurred vision, lasted about a minute, and ended with rapid recovery of consciousness. The patient sustained no significant injuries in either episode. She is concerned because one of her childhood friends passed out and died while playing football. Medical history is otherwise insignificant. The patient takes no medications and does not use alcohol or illicit drugs. She has no family history of early coronary artery disease, cardiomyopathy, or sudden cardiac death. Blood pressure is 110/70 mm Hg while supine and 108/70 mm Hg while standing. Physical examination findings are within normal limits. ECG reveals no abnormalities. Complete blood count and serum chemistries are within normal limits. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 35 of 40
35. Question
An 88-year-old woman comes to the office due to dyspnea with exertion and nocturia. The patient has had these symptoms for 6 months, and they have been slowly worsening. She has had no chest pain, palpitations, or syncope. The patient has a history of chronic hypertension and takes lisinopril. Blood pressure is 150/80 mm Hg, pulse is 80/min and regular, and respirations are 16/min. BMI is 34 kg/m2. On examination, jugular venous pressure is 10 cm H2O. The lungs are clear. Cardiac examination shows a regular rate and rhythm with no murmurs. The abdomen is mildly distended with no tenderness, and there is 2+ pitting edema in the legs. Brain natriuretic peptide (BNP) concentration is 776 pg/mL and D-dimer is normal. Chest x-ray reveals no cardiomegaly, no pulmonary edema, and normal interstitial markings. What is the best next step in management of this patient?
CorrectIncorrect -
Question 36 of 40
36. Question
A 64-year-old man comes to the emergency department due to substernal chest pressure for the past 2 hours and associated mild nausea. Two weeks ago, he underwent right coronary artery stenting for stable angina that was refractory to medical therapy. The patient also has hypertension and hyperlipidemia. Blood pressure is 88/60 mm Hg and pulse is 48/min. He is diaphoretic and his extremities are cold. The lungs are clear on auscultation. There are no heart murmurs. ECG shows sinus bradycardia with 2-mm ST-segment elevations in leads II, III, and aVF. Which of the following additional factors of the patient’s history would be most helpful in diagnosing the cause of his current condition?
CorrectIncorrect -
Question 37 of 40
37. Question
A 20-year-old man develops substernal chest pain and palpitations, followed by brief syncope while playing soccer. The patient is rushed to the emergency department where he reports feeling fine. He describes previous episodes of “chest pressure” while overexerting himself, after which he needs to stop and rest. He has had no previous episodes of syncope. Medical history is unremarkable. The patient does not use tobacco, alcohol, or illicit drugs. There is no family history of coronary heart disease or sudden death. Blood pressure is 122/78 mm Hg and pulse is 78/min. Cardiac examination reveals no murmurs in both the supine and standing positions. ECG shows normal sinus rhythm with a rate of 72/min. No ST-segment or T-wave abnormalities are present. The QTc interval is 410 msec. The patient is recommended to avoid exercise until he can undergo further workup, but 2 days later he collapses and dies while jogging. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 38 of 40
38. Question
A 23-year-old man is evaluated for a murmur discovered at a health fair. His past medical history is insignificant, and he feels well with no cardiac symptoms. The patient plays soccer and jogs regularly. His immediate family is healthy. Blood pressure is 122/70 mm Hg and pulse is 72/min. A 2/6 midsystolic murmur is heard at the left sternal border. The femoral pulses are full, and there is no brachial-femoral pulse delay. Echocardiography shows bicuspid aortic valve with a mildly increased gradient and no dilation of the aortic root. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 28-year-old woman comes to office due to progressive fatigue and dyspnea on exertion over the last year. The patient can only walk 2 flat city blocks before stopping for breath. She also reports occasional episodes of near-syncope when coughing or defecating. The patient has no other medical conditions. She is a former smoker and does not drink alcohol. The patient lives with her boyfriend in the city and continues to work part-time as a professional violinist. Temperature is 36.7 C (98.1 F), blood pressure is 102/65 mm Hg, pulse is 85/min, and respirations are 16/min. Pulse oximetry on room air is 93% at rest and 85% with exertion. BMI is 19 kg/m2. The patient’s 6-minute walking distance is 390 m (normal: >500 m). Complete blood count, renal function, and plasma electrolytes are within normal limits. Transthoracic echocardiography reveals right ventricular hypertrophy with reduced systolic function, moderate tricuspid regurgitation, and an elevated pulmonary artery systolic pressure of 63 mm Hg. Further evaluation reveals no secondary causes of pulmonary hypertension. In addition to initiating supplemental oxygen and pulmonary vasodilator therapy, which of the following recommendations best applies to this patient at this time?
CorrectIncorrect -
Question 40 of 40
40. Question
A 24-year-old man is evaluated for fatigue and palpitations. He reports good exercise tolerance with only mild dyspnea on exertion. Electrocardiogram shows normal sinus rhythm with a right bundle branch block. Right and left cardiac catheterization is obtained and the following blood oxygen saturation values are reported:
Superior vena cava
55%
Inferior vena cava
60%
Right atrium
57%
Right ventricle
74%
Pulmonary artery
72%
Left ventricle
99%
Aorta
98%
Which of the following is the most likely physical examination finding in this patient?
CorrectIncorrect
