Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
The following vignette applies to the next 2 items.
A 25-year-old man comes to the office with a 2-month history of palpitation, sweating, and heat intolerance. The patient has no diplopia, eye pain or redness, decreased vision, or neck pain. Medical history is unremarkable, and he takes no medications. Temperature is 36.7 C (98.1 F), blood pressure is 130/70 mm Hg, pulse is 115/min (regular), and respirations are 18/min. Examination shows mild lid-lag but no conjunctival erythema or proptosis. Extraocular movements are intact. Mild, diffuse, nontender enlargement of the thyroid gland is noted. Neurologic examination demonstrates a fine hand tremor and brisk symmetric reflexes but is otherwise unremarkable. Laboratory tests show a normal complete blood count and basic metabolic profile. Results of thyroid function tests are as follows:
TSH
<0.01 μU/mL
Free T4
2.5 ng/dL (normal: 0.8-1.9)
Total T3
250 ng/dL
Radioactive iodine uptake at 24 hours is 36% (normal: 8%-25%), and the scan shows a diffuse uptake pattern. Serum thyroid-stimulating immunoglobulin level is mildly elevated.
Item 1 of 2
Which of the following is the best next step in management of this patient?CorrectIncorrect -
Question 2 of 40
2. Question
Item 2 of 2
Appropriate treatment is initiated. Four weeks later, the patient returns to the office and says that his symptoms have resolved. Blood pressure is 120/80 mm Hg and pulse is 82/min. Eye examination shows no lid-lag. The thyroid examination is unchanged, and the rest of the examination is unremarkable. Which of the following is the best next step in management?CorrectIncorrect -
Question 3 of 40
3. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 61-year-old man comes to the office for follow-up of long-standing type 2 diabetes mellitus. Treatment currently consists of metformin, dietary modification, and regular exercise. On his current regimen, the patient’s weight has been mostly stable over the last 2 years, but he has noticed some weight loss in the last 6 weeks. He also has mild constipation but no abdominal pain, nausea, or excessive urination. Medical history is significant for hyperlipidemia and hypertension, for which he takes atorvastatin, amlodipine, and valsartan. He also takes low-dose aspirin and a daily multivitamin. The patient does not drink alcohol but has a 45-pack-year smoking history. His father had type 2 diabetes mellitus and died of a stroke, and his mother had thyroid cancer that required surgery. Blood pressure is 134/80 mm Hg and pulse is 88/min. BMI is 30 kg/m2. Neck examination is normal. Lungs are clear to auscultation. Abdominal examination reveals no masses or tenderness. Laboratory results are as follows:
Calcium
12.1 mg/dL
Glucose
120 mg/dL
Albumin
4.0 g/dL
Hemoglobin A1c
7.0%
Six months ago, his chemistry profile was normal.
Item 1 of 2
Which of the following is the best next step in evaluation of this patient?
CorrectIncorrect -
Question 4 of 40
4. Question
Item 2 of 2
The patient is scheduled for additional testing but is unable to return for evaluation. About 2 weeks after his visit, he is brought to the emergency department due to weakness, nausea, increased urination, and progressive constipation. Blood pressure is 90/70 mm Hg and pulse is 110/min. Mucous membranes are dry. Laboratory results show a serum parathyroid hormone level of 9 pg/mL, serum calcium of 14.1 mg/dL, and serum creatinine of 2.6 mg/dL. Which of the following is the most likely cause of this patient’s hypercalcemia?
CorrectIncorrect -
Question 5 of 40
5. Question
The following vignette applies to the next 2 items
A 30-year-old woman comes to the office due to tingling and numbness in both of her distal lower extremities for the last 3 months. Her symptoms are gradually worsening. She also has had intense fatigue. She has not had any weight change, constipation, skin dryness, headaches, or visual changes. The patient was diagnosed with primary hypothyroidism secondary to Hashimoto thyroiditis when she was 10 years old. She is currently on 100 mcg per day of levothyroxine orally. Her mother also has hypothyroidism. The patient does not use tobacco, alcohol, or recreational drugs. Her menstrual cycles have been irregular for the last 6 months. Her last menstrual period was 2 months ago. She is sexually active with one partner. Blood pressure is 114/78 mm Hg and pulse is 72/min. She weighs 69 kg (152 lbs) and is 163 cm (5’4″) tall. Her thyroid is nonpalpable. Her mucous membranes are moist and pale. Her tongue appears to be bald. She does not have any scleral icterus. Vibration and proprioception are decreased in both of her lower extremities distally. Pain and temperature sensations appear normal. Her ankle jerks are absent, but other reflexes are brisk. Babinski is present, and Romberg signs is positive. The rest of the physical examination is unremarkable. Stool obtained from the rectal examination is negative for occult blood. Laboratory results reveal a hemoglobin of 8 g/dL and hematocrit of 24%. Her total leukocyte count is 3,200/mm3. Her platelet count is 300,000/mm3. Basic serum chemistries are within normal limits. Her total T4 level is 8.2 mcg/dL (normal 4-12 mcg/dL) and TSH level is 2.4 micro IU/mL.
Item 1 of 2
What is the next best step in the management of this patient?
CorrectIncorrect -
Question 6 of 40
6. Question
Item 2 of 2
Which of the following is most crucial to monitor during the first few days of treatment in the above patient?
CorrectIncorrect -
Question 7 of 40
7. Question
The following vignette applies to the next 2 items
A 40-year-old woman comes to the clinic after noticing a small swelling in the front of her neck. She has no pain, dysphagia, hoarseness, or difficulty breathing. She also has no hyper- or hypothyroid symptoms such as heat or cold intolerance, fatigue, or weight changes. Physical examination shows a mobile nodule in her left thyroid lobe. The patient has no history of neck irradiation or family history of thyroid illness. She currently takes no medications. The rest of the physical examination is unremarkable.
Item 1 of 2
Which of the following is the best next step in evaluation of this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
Item 2 of 2
After performing the appropriate investigation, a diagnosis of papillary thyroid cancer is made. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 9 of 40
9. Question
A 26-year-old woman comes to the office due to fatigue and poor sleep. For the past month, she has felt unusually tired and has been unable to keep up with her usual aerobics classes. Prior to the onset of symptoms, the patient began taking over-the-counter “energy” pills to improve stamina and promote weight loss. She wants to lose weight because she is getting married in a few months. Medical history is unremarkable; family history is also insignificant. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 138/66 mm Hg and pulse is 101/min. A resting hand tremor is noted. Ocular examination is normal. The thyroid gland is not palpable and there is no neck tenderness. The remainder of the physical examination is unremarkable. Thyroid function tests show TSH of <0.01 μU/mL and free T4 of 2.3 ng/dL (normal: 0.9-1.7). Which of the following is most likely to be found on further evaluation of this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 10 of 40
10. Question
A 29-year-old woman comes to the office for evaluation of hypercalcemia. Her serum calcium was 12.1 mg/dL on routine laboratory investigations performed for a life insurance application. The patient feels well and has had no excessive urination, bone pain, abdominal pain, headache, or constipation. Medical history is significant for upper gastrointestinal hemorrhage a year ago; the bleed was due to a large gastric ulcer, for which she is currently taking an oral proton pump inhibitor. She has a 10-pack-year smoking history but does not use alcohol or illicit drugs. The patient’s menstrual cycles are regular; she has never been pregnant, is sexually active with one partner, and uses barrier contraception to prevent pregnancy. The patient’s mother underwent parathyroid surgery for symptomatic hypercalcemia and takes a pill twice a week for an unspecified pituitary tumor. Blood pressure is 128/80 mm Hg and pulse is 78/min. BMI is 27 kg/m2. Neck examination is unremarkable. A few small subcutaneous lipomas are present on the patient’s back. The rest of her physical examination is unremarkable. Laboratory results are as follows:
Serum chemistries
Calcium
12.0 mg/dL
Phosphorus
1.9 mg/dL
Creatinine
0.8 mg/dL
Parathyroid hormone
718 pg/mL
25-hydroxyvitamin D
31 ng/mL (normal: 30-50 ng/mL)
24-hour urine calcium
415 mg
Bone mineral density by DXA is normal. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 11 of 40
11. Question
The following vignette applies to the next 2 items.
A 16-year-old girl is brought to the physician by her parents. Her mother is concerned because the girl has lost 10 pounds in the last 3 months. She constantly feels weak and tired. She is doing well in high school. The patient says that she eats well, although her appetite has decreased. Her last menstrual period was 3 months ago. She is not sexually active. She does not use tobacco, alcohol, or illicit drugs. Physical examination shows a young, thin girl with multiple brown freckles. The patient has a decreased amount of axillary and pubic hair for her age. Patchy brown spots are seen on her lips and buccal mucosa. Mild generalized muscular tenderness is present. She appears well-groomed, alert, and communicative and does not appear to be especially anxious. Her parents, on the other hand, are worried about her condition and want to know her diagnosis.
Item 1 of 2
Which of the following is the most appropriate statement regarding this patient’s case?
CorrectIncorrect -
Question 12 of 40
12. Question
Item 2 of 2
The patient returns with her parents for a follow-up visit. She complains of intermittent abdominal pain during the past week. Examination findings remain unchanged from the previous visit. Laboratory results are as follows:
Complete blood count Hemoglobin 12.8 g/dL Hematocrit 39% Platelets 315,000/µL Leukocytes 5,500/µL Segmented neutrophils 62% Lymphocytes 30% Monocytes 8% Serum chemistry Serum Na 132 mEq/L Serum K 5.2 mEq/L Chloride 107 mEq/L Bicarbonate 20 mEq/L Blood urea nitrogen 18 mg/dL Serum creatinine 0.9 mg/dL Calcium 10.1 mg/dL Glucose 70 mg/dL Urinalysis is normal. Pregnancy test is negative. Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 13 of 40
13. Question
A 76-year-old woman is brought to the emergency department due to altered mental status. Before admission, she had lived independently and had no contact with her family or primary care physician for several months. Past medical history includes type 2 diabetes mellitus, hypertension, and osteoporosis, but she has no history of dementia or alcohol or illicit drug use. The patient’s medications include metoprolol, glipizide, hydrochlorothiazide, and alendronate; she has been on these for several years. Her temperature is 36.7 C (98 F), blood pressure is 130/70 mm Hg, pulse is 105/min, and respirations are 16/min. Pulse oximetry is 97% on room air. Examination shows a drowsy woman in no acute distress who is disoriented to time and place. The neck is supple without thyroid enlargement. Cardiopulmonary examination is normal. Pupillary reflexes are intact, but the patient is otherwise not cooperative with neurologic examination. Laboratory studies show normal complete blood count, basic metabolic panel, and urinalysis. Chest x-ray is normal. CT scan of the head shows generalized cerebral atrophy. Lumbar puncture with cerebrospinal fluid analysis is normal. What is the most appropriate next step in evaluation of this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 38-year-old woman with a history of bipolar I disorder comes to the office due to low energy. The patient felt well until 4 months ago when she noticed she was reacting slowly at work and was reluctant to meet with friends on weekends due to fatigue. She is afraid she is becoming depressed again. The patient says, “I am so discouraged. I really felt so much better on my medication, and now I feel like I’m slipping.” She has a history of multiple hospitalizations for manic and depressive episodes since late adolescence. She attempted suicide at age 20 by taking an overdose of aspirin. The patient was previously treated with valproate and olanzapine and has been taking lithium for the past year. Her other medical issues include hypertension and allergic rhinitis, for which she takes hydrochlorothiazide and loratadine, respectively. On review of systems, the patient reports fatigue and difficulty concentrating over the past few weeks. Mental status examination shows a tired appearance and sad affect. She has no suicidal ideation. Physical examination shows no abnormalities. The patient’s blood lithium level is 0.9 mEq/L (range: 0.6-1.2 mmol/L). Other laboratory results are as follows:
Complete blood count
Hemoglobin
12.9 g/dL
Hematocrit
39%
Mean corpuscular volume
95 fL
Platelets
240,000/mm3
Leukocytes
7,500/mm3
Serum chemistry
Sodium
142 mEq/L
Potassium
4.2 mEq/L
Chloride
104 mEq/L
Bicarbonate
28 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.8 mg/dL
Glucose
93 mg/dL
Calcium
9.1 mg/dL
Liver function studies
Alkaline phosphatase
52 U/L
Aspartate aminotransferase (SGOT)
18 U/L
Alanine aminotransferase (SGPT)
20 U/L
Endocrine
TSH
14 µU/mL
Free T4
0.4 ng/dL (normal: 0.9-2.4 ng/dL)
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
A 41-year-old woman comes to the physician with an 8-month history of amenorrhea. Multiple home pregnancy tests during this time have been consistently negative. She has mild dyspareunia and blurred vision but no headaches, galactorrhea, hot flashes, or weight change. The patient’s past medical and family histories are unremarkable. She takes no medications, including over-the-counter drugs. She does not use alcohol, tobacco, or intravenous drugs. Physical examination is unremarkable. Basic metabolic panel and complete blood count are within normal limits. Her hormone profile shows a prolactin level of 50 ng/mL (normal 5-20 ng/mL). Serum luteinizing hormone level is undetectable, follicle-stimulating hormone is low normal, and the α-subunit is markedly increased. Serum thyroid-stimulating hormone, testosterone, and insulin-like growth factor 1 are normal. Magnetic resonance imaging of the pituitary shows a 2-cm pituitary tumor with suprasellar extension. What is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 16 of 40
16. Question
A 36-year-old woman comes to the office due to a 5-month history of progressive lower back pain. The pain is aching and nonradiating and has no aggravating or relieving factors. Two years ago, the patient underwent Roux-en-Y gastric bypass surgery for morbid obesity, after which she lost 45.4 kg (100 lb). She follows a normal diet and takes a daily multivitamin containing calcium (1,200 mg of elemental calcium) and vitamin D (400 IU of cholecalciferol). Spinal examination shows no focal tenderness. Laboratory results are as follows:
Serum creatinine
1.0 mg/dL
Calcium
9.1 mg/dL
Alkaline phosphatase
155 U/L
Serum phosphorus
2.2 mg/dL
Parathyroid hormone
955 pg/mL
Bone mineral density by DXA reveals a T-score of −2.0 at the lumbar spine and −1.5 at the hip. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 17 of 40
17. Question
A 35-year-old woman comes to the emergency department due to a “racing heart” and shortness of breath. She has had insomnia and increasing anxiety for the past several weeks. The patient has no prior medical problems and takes no medications. She has no drug allergies and does not use tobacco, alcohol, or illicit drugs. Blood pressure is 140/70 mm Hg and pulse is 120/min. Physical examination shows a diffusely enlarged, warm thyroid gland. There is a fine tremor in her outstretched hands. ECG shows sinus tachycardia. Serum TSH is decreased and free thyroxine (T4) is increased. The patient is treated with multiple drugs, including propranolol. In addition to its beta-adrenergic receptor-blocking activity, this drug is likely to decrease which of the following?
CorrectIncorrect -
Question 18 of 40
18. Question
The following vignette applies to the next 2 items
A 64-year-old woman comes to the physician because she has had bilateral foot numbness and burning for the past three months. The symptoms are especially bothersome at night. She has a history of hypertension, coronary artery disease, and type 2 diabetes mellitus. She had an anterior wall myocardial infarction two years ago, which was treated with angioplasty and stenting of the left anterior descending artery. An echocardiogram obtained one year ago revealed an ejection fraction of 40%. She does not use tobacco, alcohol, or drugs. Her medications include metoprolol, furosemide, glyburide, atorvastatin, aspirin, and enalapril. She has been on oral hypoglycemic medications for the last ten years. Her blood pressure is 142/82 mmHg and her heart rate is 63/min. Her BMI is 34 kg/m2. Physical examination shows intact skin over both feet and 2+ peripheral pulses.
Item 1 of 2
Which of the following is the most appropriate next step in managing this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
Item 2 of 2
The patient returns two months later for follow-up. She has persistent symptoms and complains of poor sleep. Her last HbA1c was 7.9% and creatinine was 0.9 mg/dL. Urinalysis shows trace proteinuria. Which of the following is the best management option for this patient?
CorrectIncorrect -
Question 20 of 40
20. Question
The following vignette applies to the next 3 items.
A 29-year-old man comes to the emergency department complaining of palpitations, sweating, and severe headache. His symptoms resolve spontaneously by the time he is evaluated. He has had at least 2 similar episodes during the past 2 months. The patient’s family history is unremarkable. He does not use tobacco, alcohol, or illicit drugs. His primary care provider saw him after the first episode and prescribed an anxiolytic medication. However, the patient felt drowsy at his job and stopped the medication. Physical examination shows a thin man who appears anxious and diaphoretic. The thyroid is normal to palpation without any obvious nodules. His temperature is 36.7 C (98 F), blood pressure is 126/84 mm Hg, pulse is 86/min, and respirations are 16/min. During his prior emergency department visit for an identical episode, his blood pressure was 150/100 mm Hg and pulse was 120/min. The laboratory results at that time showed normal thyroid function tests.
Item 1 of 3
Which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 21 of 40
21. Question
Item 2 of 3
Endocrine studies yield results highly suspicious of a neuroendocrine tumor. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 22 of 40
22. Question
Item 3 of 3
The patient is placed on appropriate preoperative medications and is taken for surgical removal of the tumor. During the procedure, he rapidly becomes hypotensive. His blood pressure falls from 110/89 mm Hg to 80/50 mm Hg. Which of the following is the most appropriate therapy for this patient’s hypotension?
CorrectIncorrect -
Question 23 of 40
23. Question
A 31-year-old woman, gravida 1 para 1, comes to the office 5 weeks after an uneventful vaginal delivery. The patient has fatigue, sweating, and heat intolerance. She has had no skin rash, headache, vision changes, or ocular symptoms, and her appetite is normal. The patient is not breastfeeding because her milk supply rapidly diminished. She has not yet resumed normal menstruation. Medical history is unremarkable, and her only medication is a daily prenatal vitamin that she continued following delivery. The patient’s mother has hypothyroidism and celiac disease. Blood pressure is 121/67 mm Hg and pulse is 109/min. Examination shows an enlarged, nontender thyroid gland with no nodules. Ocular examination shows mild lid lag without proptosis. The remainder of the examination is unremarkable. Laboratory results are as follows:
TSH
<0.01 μU/mL
Total T4
18 μg/dL
Anti–thyroid peroxidase antibody
23 IU/mL (normal: <9)
Serum thyroglobulin
57 ng/mL (normal: <33)
The radioactive iodine uptake in the thyroid gland is 1.5% at 24 hours (normal: 8%-25%). Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 24 of 40
24. Question
A 35-year-old woman comes to the office due to hot flashes. Her last menstrual period was a year ago, and she began having hot flashes 4 months ago. The patient’s symptoms have become progressively worse and are starting to interfere with sleep and normal daily activities. Medical history is notable for Hodgkin lymphoma, for which she underwent treatment with chemotherapy and radiation 18 months ago. Family history is unremarkable. The patient lives with her husband and 2 children, and underwent a tubal ligation after the delivery of her second child 5 years ago. She does not use tobacco or alcohol. Current medications include calcium and vitamin D supplements. Blood pressure is 110/70 mm Hg and pulse is 80/min. BMI is 19 kg/m2. Physical examination, including breast and pelvic examination, is unremarkable. Laboratory results show a normal complete blood count and basic metabolic panel. LH is 25 mU/mL (normal, 3-20 mU/mL) and FSH is 56 mU/mL (normal, 0.8-13 mU/mL). Bone density using DXA reveals a Z-score of -2.5 at the lumbar spine and -1.7 at the hip. Which of the following is the most appropriate treatment for this patient?
CorrectIncorrect -
Question 25 of 40
25. Question
A 44-year-old woman comes to the office for follow-up of a vertebral compression fracture. Three weeks ago, she slipped and fell on a wet kitchen floor and developed severe lower back pain. Lumbar x-ray in the emergency department revealed a mild L1 compression fracture. She was given analgesics and instructed to follow up with her physician. The patient’s pain is adequately controlled, and she has no other symptoms. Medical history is significant for prophylactic bilateral mastectomy and salpingo-oophorectomy at age 35 due to BRCA mutation. Apart from a daily vitamin D and calcium supplement, which she started taking following her fracture, the patient takes no medications. Vital signs and physical examination are normal. Laboratory test results, including blood counts, calcium, phosphorus, renal and hepatic markers, vitamin D, and TSH, are within normal limits. Bone mineral density testing with DXA reveals a T-score of −1.9 at the lumbar spine and −1.8 at the hip. The patient is counseled on optimizing her diet and initiating regular weight-bearing exercise when appropriate. Which of the following additional interventions is indicated at this time?
CorrectIncorrect -
Question 26 of 40
26. Question
A 60-year-old woman comes to the office for follow-up of type 2 diabetes mellitus. She has been taking metformin for the past 2 years with a gradual rise in hemoglobin A1c. Medical history includes hypertension and diabetic nephropathy with moderately increased albuminuria. In addition to metformin, her medications include lisinopril and atorvastatin. Blood pressure is 136/90 mm Hg and pulse is 76/min. BMI is 37 kg/m2. Laboratory results are as follows:
Serum chemistry
Glucose
165 mg/dL
Sodium
140 mEq/L
Potassium
4.1 mEq/L
Blood urea nitrogen
22 mg/dL
Creatinine
1.0 mg/dL
Estimated glomerular filtration rate
64 mL/min/1.73 m2
Hemoglobin A1c
8.2%
Treatment with canagliflozin is started. Which of the following metabolic effects is most likely to occur due to treatment in this patient?
CorrectIncorrect -
Question 27 of 40
27. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 31-year-old man with type 1 diabetes mellitus is brought to the emergency department due to abdominal discomfort, nausea, and vomiting. He has not felt well for the past 2 days and has had intractable vomiting. The patient stopped taking his regular dose of insulin because he was unable to “hold anything down.” Initial laboratory results show positive serum ketones, blood glucose of 360 mg/dL, and blood pH of 7.17. In the emergency department, he is started on intravenous normal saline with potassium and a continuous insulin infusion. Five hours after admission to the intensive care unit, he feels better. Laboratory results are as follows:
Sodium
133 mEq/dL
Potassium
3.6 mEq/dL
Bicarbonate
14 mEq/L
Chloride
98 mEq/L
Blood urea nitrogen
24 mg/dL
Creatinine
1.3 mg/dL
Blood glucose
180 mg/dL
Item 1 of 2
Which of the following is the best next step in management of this patient?CorrectIncorrect -
Question 28 of 40
28. Question
Item 2 of 2
Ten hours after admission, the patient feels better. He has had no vomiting over the last several hours, and his abdominal discomfort has subsided. He is tolerating oral fluid. The patient is currently on an insulin infusion and intravenous fluids. Repeat laboratory results are as follows:Sodium
138 mEq/dL
Potassium
3.8 mEq/dL
Bicarbonate
18 mEq/L
Chloride
112 mEq/L
Blood urea nitrogen
14 mg/dL
Creatinine
0.9 mg/dL
Blood glucose
154 mg/dL
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 29 of 40
29. Question
A 53-year-old woman with a 10-year history of chronic autoimmune hypothyroidism (Hashimoto thyroiditis) is evaluated for a monthlong history of fatigue. The patient has also been feeling colder than usual and has noticed a significant decrease in the frequency of bowel movements. She has had no changes in weight or physical activity level. The patient is adherent with levothyroxine and has had no dose changes for the past 5 years. Medical history is significant for a hiatal hernia and gastroesophageal reflux disease. She began taking pantoprazole 6 months ago. The patient experienced menopause 2 years ago. Temperature is 36.2 C (97.2 F), blood pressure is 145/80 mm Hg, and pulse is 60/min. On physical examination, the thyroid is not enlarged or tender. The remainder of the physical examination is normal. Serum TSH is 14.8 U/L but was 4.9 U/L 4 months ago. Which of the following is the most likely underlying cause of this patient’s current symptoms?
CorrectIncorrect -
Question 30 of 40
30. Question
A 52-year-old woman comes to the office for follow-up of type 2 diabetes mellitus. The patient was diagnosed with diabetes 6 months ago and initiated intensive lifestyle modification with increased exercise and a calorie-restricted diet; since that time, she has felt better subjectively but has lost only 2 kg (4.4 lb). Vital signs are normal. BMI is 35 kg/m2. Fasting glucose is 155 mg/dL and hemoglobin A1c is 8.0%. Serum renal and liver function markers are normal. After discussion with the patient, metformin therapy is initiated. Which of the following physiologic changes are most likely to result as a direct effect of this medication?
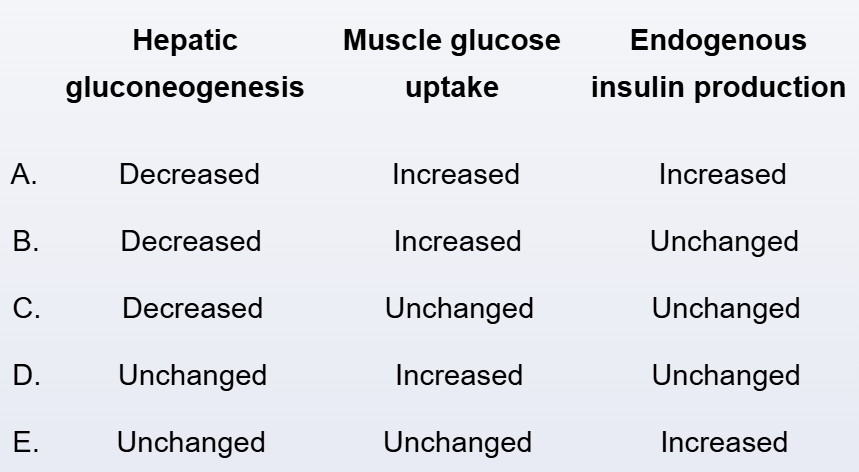 CorrectIncorrect
CorrectIncorrect -
Question 31 of 40
31. Question
A 56-year-old woman comes to the physician with lethargy, weight loss, nausea, vomiting, and constipation for the past 2 months. She is 3 years postmenopausal and has no long-standing medical problems. The patient currently takes no prescription medications and does not use tobacco or alcohol. Her family history is positive for osteoporosis and hypertension. Her blood pressure is 124/66 mm Hg and pulse is 64/min. She weighs 63 kg (138 lb) and is 160 cm (5′ 3″) tall. Her body mass index is 24.4 kg/m2. The patient appears mildly pale. The thyroid gland is normal to palpation. Heart and lung sounds are normal. Abdominal examination is unremarkable. Neurologic examination shows prolonged relaxation time of the ankle reflexes. Laboratory results are as follows:
Hemoglobin
11.2 g/dL
Sodium, serum
129 mEq/L
Glucose, serum
64 mg/dL
Prolactin, serum
15 ng/mL (normal 5-20 ng/mL)
Thyroid-stimulating hormone
0.35 µU/mL
Free T4
0.5 ng/L
Red blood cells are normochromic and normocytic. The 8:00 AM serum cortisol is 7 µg/dL (normal 5-20 µg/dL). Repeat thyroid function tests show similar results.
Which of the following is the most appropriate next step in evaluation of this patient?
CorrectIncorrect -
Question 32 of 40
32. Question
An 83-year-old woman with mild cognitive impairment comes to the office due to a feeling of “not being myself.” The patient has lived in an assisted living facility since her husband died 2 years ago. She is accompanied by a caregiver, who notes that the patient has developed progressive changes in behavior and personality over the last several months. The patient has often refused meals and snacks and has had decreased participation in group activities that she previously enjoyed. She also gets agitated very easily and often “wants to be left alone.” Medical history is notable for hypertension, heart failure with preserved ejection fraction, and osteoporosis. The patient was also diagnosed with atrial fibrillation 6 months ago, and apixaban and escalating doses of metoprolol succinate were prescribed. She has never used tobacco, alcohol, or illicit drugs. Temperature is 37.4 C (99.3 F), blood pressure is 150/60 mm Hg, pulse is 92/min, and respirations are 22/min. Oxygen saturation is 97% on room air. Weight is 68.7 kg (151.5 lb); a month ago, it was 72.3 kg (159.4 lb). Ocular examination is normal. There is no nuchal rigidity or thyroid enlargement. The heart has an irregularly irregular rhythm, and the chest is clear to auscultation. No focal neurologic deficits are present and the patient’s gait appears stable. Laboratory tests show normal complete blood count, serum chemistry panel, and urinalysis. ECG shows atrial fibrillation with nonspecific T-wave abnormalities. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 33 of 40
33. Question
A 16-year-old boy is evaluated by the medical team in the intensive care unit. He was admitted 3 weeks ago following a motor vehicle accident. The patient sustained a C5-C6 fracture with dislocation, which resulted in quadriplegia. He currently has a tracheostomy tube and requires mechanical ventilation, and is being fed by a percutaneous endoscopic gastrostomy tube. A week ago, the patient was diagnosed with ventilator-associated pneumonia, which is being treated with piperacillin-tazobactam. His mother says that before his injury he was trying to “build up his muscles” by drinking protein shakes and taking creatine supplements. Medical history is otherwise unremarkable. The patient’s mother has Graves disease and his father has hypertension. He has no siblings. Blood pressure is 124/70 mm Hg and pulse is 64/min. Coarse crackles are heard at the right lung base. Laboratory results are as follows:
Calcium
12.8 mg/dL
Albumin
2.5 g/dL
Phosphorus
3.2 mg/dL
Parathyroid hormone
8 pg/mL (normal: 10-65 pg/mL)
25-hydroxyvitamin D
32 ng/mL (normal: 30-50 ng/mL)
1,25-dihydroxyvitamin D
14 pg/mL (normal: 15-60 pg/mL)
Repeat testing confirms these values. Ionized calcium level is 6.6 mg/dL (normal: 4-5.6 mg/dL). Which of the following is the most likely cause of this patient’s hypercalcemia?
CorrectIncorrect -
Question 34 of 40
34. Question
A 60-year-old Caucasian male complains of difficulty swallowing which has rapidly worsened within the last two weeks. The patient noticed a swelling on the front of his neck that started growing for the past month. He was otherwise in his normal state of health. He also complains of fevers, night sweats, and weight loss. He denies cough, dyspnea, chest pain, headache, abdominal pain, skin rashes, and urinary symptoms. His past medical history is significant for mild hypertension treated with hydrochlorothiazide, as well as a small goiter for the past 10 years. He states that his blood tests for thyroid hormone levels were normal, and he has never taken thyroid hormone preparations in the past. His family history is positive for a mother and several other family members with hypothyroidism. He has a smoking history of 15-pack-years but quit 25 years ago. He does not drink alcohol. Physical examination reveals a large, irregular, non-tender swelling over the inferior aspect of his neck. The lower margin of this swelling can not be palpated. He develops facial plethora and venous engorgement of the neck veins after raising his arms above the shoulder for 20 seconds. CBC and basic chemistries are normal. TSH is 26.0 μU/ml (normal 0.35-5.0 μU/ml) and free T4 is 0.2 μg/dl (normal 0.8 to 1.8 μg/dl). Antithyroid peroxidase antibodies are detected in very high titers. What is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 35 of 40
35. Question
A 56-year-old woman was found to have a TSH level of 0.2 μU/mL on routine laboratory testing. She has had no symptoms suggestive of thyrotoxicosis. She reports good energy level and no change in body weight. The patient has mild hypertension, for which she is on hydrochlorothiazide. Family history is negative for any thyroid disorder. She does not use tobacco or alcohol. She does not have allergies to any medications. The patient had her menopause about 3 years ago. She has never received hormone replacement therapy. She takes adequate amounts of calcium and vitamin D supplementation. Bone mineral density using dual photon absorptiometry was within normal range about 6 months ago. Examination is unremarkable, including examination of the thyroid gland. Free T4 levels and free T3 are well within normal limits. What is the next best step in this patient’s care?
CorrectIncorrect -
Question 36 of 40
36. Question
A 38-year-old woman comes to the office due to type 2 diabetes mellitus. She has been treated with metformin and dietary modification for the past 2 years, and her glycemic control has gradually worsened. Medical history includes obesity. Treatment with semaglutide is begun. The patient returns for follow-up after 3 months of treatment with the new drug, and the following results are observed:
Start of treatment
After 3 months of treatment
Hemoglobin A1c
8.2%
7.1%
BMI (kg/m2)
40.6
38.7
Which of the following is most likely contributing to the decreased BMI in this patient?
CorrectIncorrect -
Question 37 of 40
37. Question
A 38-year-old man with type 1 diabetes for the past 24 years comes to the physician due to pain in his feet. He describes burning pain in both feet involving the toes and forefoot. On examination, blood pressure is 145/86 mm Hg and pulse is 78/min. His hemoglobin A1c values in the past 2 years have ranged from 9%-10%. Which of the following statements is most accurate regarding this patient’s diabetic neuropathy?
CorrectIncorrect -
Question 38 of 40
38. Question
A 26-year-old woman comes to the physician to monitor her thyroid medication. She has a history of papillary thyroid cancer that was treated with a subtotal thyroidectomy and ablative radioiodine 3 years ago. The tumor was 2.1 cm in greatest dimension without lymph node involvement or distant metastasis. She currently takes 125 mcg of levothyroxine on an empty stomach every morning and has no current symptoms. Laboratory tests show undetectable thyroglobulin, undetectable anti-thyroglobulin antibodies, TSH of 4.8 μU/mL, and free T4 of 1.3 ng/dL (normal 0.8-1.8 ng/dL). One year ago, her total body radioactive iodine scan and neck ultrasound were unremarkable. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 47-year-old Caucasian man comes to the office for a follow-up visit. He was recently diagnosed with diabetes mellitus type 2, and was started on a low-carbohydrate diet six months ago. He also has obesity, hypertension and hyperlipidemia. He is a financial advisor. He does not use tobacco or illicit drugs, but drinks alcohol occasionally. His medications include enalapril, simvastatin and hydrochlorothiazide. Examination shows no abnormalities. His laboratory test results show the following:
Serum Chemistry
Serum Na 138 mEq/L Serum K 3.9 mEq/L Chloride 104 mEq/L Bicarbonate 25 mEq/L BUN 16 mg/dL Serum creatinine 1.0 mg/dL Calcium 9.8 mg/dL Glucose 210 mg/dL Hb1 AC 7.6% LFT
Total bilirubin 0.9 mg/dL Direct bilirubin 0.6 mg/dL Alkaline phosphatase 160 U/L Aspartate aminotransferase 65 U/L Alanine aminotransferase 70 U/L Lipid Profile
Total Cholesterol 210 mg/dL LDL Cholesterol 125 mg/dL HDL Cholesterol 30 mg/dL Triglycerides 315 mg/dL Which of the following is the most appropriate pharmacotherapy for this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 74-year-old man is brought to the emergency department after being found outside early on New Year’s morning. His medical history is unknown. Temperature is 31.5 C (88.7 F), blood pressure is 75/50 mm Hg, pulse is 55/min, and respirations are 8/min and shallow. On examination, the patient is unresponsive. Initial laboratory results are as follows:
Complete blood count
Hemoglobin
10.8 g/dL
Leukocytes
19,000/mm3
Serum chemistry
Sodium
130 mEq/L
Potassium
3.4 mEq/L
Blood urea nitrogen
30 mg/dL
Creatinine
1.2 mg/dL
Glucose
55 mg/dL
Thyroid function studies
TSH
1.3 µU/mL
Triiodothyronine (T3), serum
50 ng/dL
Thyroxine (T4), free
1.0 ng/dL (reference value 0.9-1.7 ng/dL)
Blood alcohol level is undetectable and urine drug screen is negative. Plasma cortisol and ACTH levels are normal. Chest x-ray reveals a right lower lobe infiltrate. The patient is placed on mechanical ventilation, pressor support, warm intravenous fluids, and broad-spectrum antibiotics. Blood cultures are pending. His vital signs improve rapidly with rewarming. Which of the following is the best next step in management of this patient’s thyroid abnormalities?
CorrectIncorrect
