Time limit: 0
Quiz Summary
0 of 40 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 40 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 40
1. Question
A 32-year-old woman, gravida 2 para 1, at 30 weeks gestation comes to the emergency department 30 minutes after experiencing a gush of clear fluid from the vagina. The patient initially thought she was leaking urine, but the leaking continued after she voided. She reports occasional contractions but no fever, chills, or vaginal bleeding. Fetal movements are normal. The pregnancy has been complicated by iron deficiency anemia requiring a prenatal vitamin and iron supplement. The patient has no chronic medical conditions and no surgical history. Her previous pregnancy ended in an uncomplicated term vaginal delivery. She does not use tobacco, alcohol, or recreational drugs. The patient owns a bakery, where she works 12-14 hours a day and often lifts heavy objects. Temperature is 36.7 C (98.1 F), blood pressure is 98/60 mm Hg, and pulse is 78/min. BMI is 28 kg/m2. The fetal heart rate is 150/min with moderate variability and no decelerations. Tocometry detects no contractions. The abdomen is nontender. Sterile speculum examination reveals a large pool of clear fluid that is nitrazine positive, and the cervix appears to be 1 cm dilated. Urinalysis shows trace protein. Transabdominal ultrasonography reveals a fetus in transverse lie and an amniotic fluid index of 5 cm. Which of the following is the most likely complication of this patient’s presentation?
CorrectIncorrect -
Question 2 of 40
2. Question
A 29-year-old woman, gravida 0 para 0, comes to the office for preconception counseling. The patient had been taking oral contraceptives for the past 6 years but stopped 2 months ago in anticipation of becoming pregnant. She has no chronic medical conditions or previous surgeries. The patient’s menses occur every 28 days and last for 4 days. Her menstrual flow is light and accompanied by mild cramping. Pap tests, the last of which was 2 years ago, have been normal. In addition to oral contraceptive pills, the patient takes a multivitamin daily. She has no known drug allergies and is up-to-date on all vaccinations. The patient drinks socially once a week but does not use cigarettes or recreational drugs. She is an aerobics instructor and teaches high-intensity classes for 90 minutes 5 days a week. On days that the patient does not teach, she exercises with free weights. In addition, she enjoys scuba diving on weekends and on vacations. Blood pressure is 100/60 mm Hg and pulse is 62/min. BMI is 22 kg/m2. Pelvic examination shows a retroverted, normal-sized uterus with no adnexal masses or tenderness, a closed cervix, and no vaginal discharge or bleeding. In addition to recommending prenatal vitamins, which of the following is the best advice for this patient?
CorrectIncorrect -
Question 3 of 40
3. Question
A 24-year-old primigravid woman at 36 weeks gestation comes to the office due to light-headedness and nausea at bedtime. Her pregnancy has been uncomplicated, and medical history is unremarkable. The patient takes folic acid daily but has been unable to tolerate oral iron. Blood pressure is 115/75 mm Hg when sitting, 110/70 mm Hg when standing, and 80/60 mm Hg when supine. Physical examination shows a uterus consistent in size with 36 weeks gestation. Which of the following is the most likely explanation for this patient’s hypotension while supine?
CorrectIncorrect -
Question 4 of 40
4. Question
A 30-year-old, previously healthy nulliparous woman comes to the office for an initial prenatal visit. The patient states that her last menstrual period was 4 months ago, and she has not taken an at-home pregnancy test. She shares that her abdomen has become larger and is “starting to show” and thinks she has begun feeling fetal movements. The patient has had no abnormal vaginal bleeding. She has a male partner of 3 years and lives with her sister, who is pregnant. BMI is 32 kg/m2. Blood pressure is 112/68 mm Hg and pulse is 86/min. The abdomen is soft, slightly distended, and without palpable masses. On pelvic examination, the uterus is small and nontender, and there are no cervical lesions. The remainder of the physical examination is unremarkable. Urine pregnancy testing is negative. Pelvic ultrasound reveals a thin endometrial stripe and no adnexal masses. The results are shared, and the patient is told that she is not pregnant. She says, “I don’t understand. I look and feel pregnant. There must’ve been a mistake.” Which of the following is the most appropriate initial response?
CorrectIncorrect -
Question 5 of 40
5. Question
A 34-year-old healthy woman, gravida 2 para 1, at 41 weeks gestation is admitted to labor and delivery with regular, painful contractions. The patient has a bicornuate uterus, but her prenatal course has been uncomplicated. Her first pregnancy resulted in a term cesarean delivery for persistent breech presentation. The patient became pregnant again 6 months after that delivery. For this pregnancy, the patient would like to attempt a vaginal delivery. Blood pressure is 118/78 mm Hg and pulse is 98/min. Fetal heart tracing is category I and contractions are every 2-3 minutes. The cervix is 6 cm dilated, 100% effaced, and the fetal vertex is at 0 station. After admission, the patient had epidural analgesia placed for pain management. Four hours later, the patient reaches complete (10 cm) cervical dilation. After 3 hours of pushing, the fetal head delivers but immediately retracts back against the perineum. Usual obstetric maneuvers fail to deliver the anterior shoulder. Which of the following is the greatest risk factor for this patient’s obstetric complication?
CorrectIncorrect -
Question 6 of 40
6. Question
A 37-year-old woman, gravida 1 para 0, is brought to the emergency department at 37 weeks gestation due to a severe headache unrelieved by acetaminophen. For the past several days, the patient has experienced fatigue, headaches, and blurred vision. She reports good fetal movement and has no abdominal pain, vaginal bleeding, or fluid leakage. The pregnancy has been complicated by gestational hypertension that has not required antihypertensive therapy. The patient has no other chronic medical conditions or previous surgeries. She takes a prenatal vitamin daily. Blood pressure is 170/110 mm Hg and pulse is 80/min. Fetal monitoring shows a baseline of 140/min, moderate variability, no decelerations, and no accelerations. Fundal height is 36 cm. Physical examination shows edema of the hands and face. The cervix is 1 cm dilated, 50% effaced, and −2 station. Deep tendon reflexes are 2+. Urine dipstick shows 3+ protein. Complete blood count and liver function panel are normal. Biophysical profile shows a score of 6/8 due to an amniotic fluid index of 3 cm (normal: >5) and a fetus in vertex presentation. Repeat blood pressure is 162/100 mm Hg. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 7 of 40
7. Question
A 31-year-old woman, gravida 1 para 0, at 19 weeks gestation comes to the office to discuss results of a serum alpha-fetoprotein (AFP) screening. The patient has been followed since her seventh week of pregnancy, when gestational age was confirmed with transvaginal ultrasound. Since learning that women should start taking folic acid prior to becoming pregnant to avoid congenital defects, she has been concerned about the possibility of having a baby with a neural tube defect. Because she started taking folic acid after the first trimester and one of her friends has a child with spina bifida, she requested testing of her AFP levels. The patient has no chronic medical conditions or previous surgeries. Family history is not significant. She does not use tobacco, alcohol, or illicit drugs. Vitals signs are within normal limits. The uterus is palpable below the umbilicus. Fetal heart rate is 155/min by bedside Doppler ultrasound. The serum AFP level is slightly elevated at 3.0 MoMs (normal: <2.5). A repeat AFP is elevated at 3.1 MoMs. Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 8 of 40
8. Question
A 36-year-old woman, gravida 1 para 0, at 34 weeks gestation comes to the emergency department due to 4 hours of decreased fetal movement. She has had no vaginal bleeding, contractions, or leakage of fluid. The patient reports no headaches, changes in vision, or right upper quadrant pain. Her last prenatal visit was at 16 weeks gestation; she moved from out of state at 18 weeks gestation for a new job. A maternal serum alpha-fetoprotein level performed at that visit was normal. The patient has a history of chronic back pain for which she takes a daily nonsteroidal anti-inflammatory drug. She has had no surgeries. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 160/90 mm Hg and pulse is 68/min. BMI is 30 kg/m2. Fetal heart rate shows a baseline of 140/min, moderate variability, accelerations, and no decelerations. The tocometer shows no contractions. Fundal height is 38 cm. Bedside ultrasound reveals an estimated fetal weight consistent with 36 weeks gestation and an amniotic fluid index of 30 cm. Laboratory results are as follows:
Complete blood count
Hemoglobin
11.2 g/dL
Platelets
180,000/mm3
Serum chemistry
Creatinine
0.6 mg/dL
Liver function studies
Aspartate aminotransferase (SGOT)
12 U/L
Alanine aminotransferase (SGPT)
24 U/L
Urinalysis
Protein
+2
Blood
negative
Glucose
present
Ketones
negative
Leukocyte esterase
negative
Nitrites
negative
Which of the following is the most likely cause of this patient’s ultrasound findings?
CorrectIncorrect -
Question 9 of 40
9. Question
The following vignette applies to the next 3 items.
A 29-year-old woman, gravida 2 para 0 aborta 1, at 34 weeks gestation comes to the office for a routine prenatal visit. The patient reports no abdominal pain, leakage of fluid, or vaginal bleeding. Fetal movement is normal. Since her last visit 2 weeks ago, she has developed severe pruritus on her abdomen, which has not responded to over-the-counter moisturizers. The patient has had no recent contact with anyone who has had a fever, rash, or pruritus. She was diagnosed with gestational diabetes mellitus that is well controlled with an insulin regimen. Earlier in the pregnancy, she had an episode of vulvar candidiasis that was treated with topical antifungal cream. The patient has no chronic medical conditions or previous surgeries. She takes prenatal vitamins daily and has no medication allergies. The patient does not use tobacco, alcohol, or recreational drugs. Temperature is 36.7 C (98 F) and blood pressure is 100/70 mm Hg. BMI is 31 kg/m2. Fetal heart rate is 145/min and fundal height is 35 cm. Physical examination shows prominent abdominal striae and some linear excoriations on the abdominal wall unrelated to the striae. The remainder of the skin examination is normal. Laboratory results are as follows:
Hemoglobin
10.8 g/dL
Platelets
140,000/µL
Aspartate aminotransferase
12 U/L
Alanine aminotransferase
24 U/L
Bile acids
8 µmol/L (normal: 1-9)
Item 1 of 3
Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 10 of 40
10. Question
Item 2 of 3
The patient is prescribed treatment for her symptoms. She returns a week later for follow-up and reports good fetal movement and no contractions, vaginal bleeding, or leakage of fluid. Her pruritus has worsened, and blisters have appeared near her umbilicus and are spread out over her abdomen. Temperature is 36.7 C (98 F) and blood pressure is 100/70 mm Hg. Fetal heart rate is 145/min and fundal height is unchanged at 35 cm. Physical examination reveals the following:

Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 11 of 40
11. Question
Item 3 of 3
Which of the following is the best next step in treatment of this patient?
CorrectIncorrect -
Question 12 of 40
12. Question
A 25-year-old woman, gravida 2 para 1, comes to the office at 28 weeks gestation for her initial prenatal visit. She is known to be Rh(D)-negative, and her husband is Rh(D)-positive. Her previous pregnancy was uncomplicated, with no episodes of bleeding prior to delivery. The patient’s labor was complicated by a significant intrapartum abruptio placentae, although she ultimately had a vaginal delivery. She received the same standard dose of anti-D immune globulin at 28 weeks gestation and immediately postpartum. She did not require a blood transfusion and recovered with iron supplementation. Prior to this visit, the patient came to the emergency department due to cramping without bleeding, and a transvaginal ultrasound at that time was consistent with 8 weeks gestation. Today, she has no vaginal bleeding, leakage of fluid, or contractions; fetal movements are occasional. She has no chronic medical problems and no surgical history. Temperature is 36.7 C (98 F), blood pressure is 100/70 mm Hg, and pulse is 80/min. Fundal height is 30 cm. Fetal heart rate is 145/min. Routine blood work shows that anti-D antibody titers are 1:32. Which is the most likely explanation for the positive antibody results in this patient?
CorrectIncorrect -
Question 13 of 40
13. Question
A 39-year-old woman, gravida 3 para 2, at 7 weeks gestation comes to the emergency department for vaginal bleeding that began 3 hours ago and has soaked through a pad. Since her arrival, the bleeding has subsided. She reports no abdominal pain or cramping. Her first prenatal visit is in 1 week. The patient has a history of HIV, contracted 3 years ago through unprotected sexual intercourse, but she has declined treatment as she has felt “healthy.” She has no previous surgeries. The patient’s 2 prior pregnancies ended in uncomplicated term vaginal deliveries; the last delivery was 4 years ago. Her last Pap test, 4 years ago, was normal. She has smoked half a pack of cigarettes a day for 13 years but does not drink alcohol or use illicit drugs. Blood pressure is 130/80 mm Hg and pulse is 82/min. BMI is 24 kg/m2. Abdominal examination shows no tenderness or masses. The external genitalia have no lesions. Speculum examination reveals minimal bright red blood in the vaginal vault. The cervix is closed and there is a 3-cm, firm, white, irregular mass on the anterior cervix that bleeds when touched with a cotton applicator. Laboratory results are as follows:
Blood type
O, Rh positive
Hemoglobin
11.2 g/dL
β-hCG
4,027 IU/L
CD4+ count
165/mm3
HIV-1 viral load
44,500 copies/mL
A bedside transvaginal ultrasound reveals an intrauterine gestation with normal fetal cardiac activity. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 14 of 40
14. Question
A 16-year-old girl, gravida 1 para 0, at 40 weeks gestation comes to labor and delivery with her mother due to several hours of contractions and increasing pelvic pressure. The patient’s pregnancy has been uncomplicated. She has no chronic medical conditions and has had no previous surgeries. The patient takes a daily prenatal vitamin and does not use tobacco, alcohol, or recreational drugs. Vital signs are normal. Fetal heart rate tracing is category 1. Tocodynamometer shows contractions every 2-3 minutes. On digital cervical examination, the cervix is 10 cm dilated, with the fetal head at −1 station and in occiput anterior position. The patient is admitted and declines epidural analgesia. She is instructed to begin pushing, and an hour later, she receives oxytocin to increase the strength and frequency of the contractions. Despite 3 hours of correct pushing technique, significant maternal effort, and adequate contractions, the fetal vertex does not descend past −1 station and is not engaged. Fetal heart rate monitoring continues to show a category 1 tracing. The patient feels fatigued, but her mother encourages her to continue pushing. In most states, which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 15 of 40
15. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 36-year-old woman, gravida 3 para 2, at 32 weeks gestation comes to the emergency department due to abdominal pain. The patient’s symptoms started a day ago as mild right-sided abdominal pain. Since then, the pain has become increasingly severe and is accompanied by fever, heartburn, and diarrhea. The patient has had no contractions, vaginal bleeding, or leakage of fluid. Fetal movement is normal. The pregnancy has been uncomplicated. She has no chronic medical conditions and has had no surgeries. The patient takes a daily prenatal vitamin and does not use tobacco, alcohol, or illicit drugs. Temperature is 38.9 C (102 F), blood pressure is 140/80 mm Hg, and pulse is 112/min. Fetal heart rate monitor shows a baseline of 160/min, moderate variability, and no decelerations. Tocometry shows no contractions. Cardiopulmonary examination reveals tachycardia but a regular rhythm and no rubs. The lungs are clear to auscultation. Abdominal examination reveals tenderness throughout the right lower quadrant and flank but no uterine fundal or costovertebral angle tenderness. There is no rebound or guarding. McBurney point is nontender. Pelvic examination reveals no adnexal masses or tenderness. Laboratory results are as follows:
Hemoglobin
10.8 g/dL
Leukocytes
13,000/mm3
Item 1 of 2
Which of the following is the best next step in diagnosing this patient’s condition?
CorrectIncorrect -
Question 16 of 40
16. Question
Item 2 of 2
Inadequate treatment would put this patient at increased risk for which of the following complications?
CorrectIncorrect -
Question 17 of 40
17. Question
A 36-year-old woman, gravida 1 para 0, at 10 weeks gestation comes to the office for her initial prenatal visit. The patient has had mild nausea throughout the pregnancy but can tolerate small meals. She reports no vaginal bleeding or cramping. The patient’s partner has a history of male factor infertility due to low sperm count; this pregnancy is the result of an intrauterine insemination. She has no chronic medical conditions or previous surgeries. The patient has no history of abnormal Pap testing; her last Pap test was 2 years ago. She has a history of gonococcal cervicitis at age 23 but there was no evidence of tubal blockage during her infertility evaluation. The patient takes a prenatal vitamin, folic acid, and vitamin B6 daily. She works as a high school history teacher and volleyball coach. Family history is noncontributory. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 98/60 mm Hg and pulse is 74/min. BMI is 23 kg/m2. Cardiopulmonary examination is unremarkable. Pelvic examination reveals normal external genitalia, minimal physiologic cervical discharge throughout the vaginal vault, and a cervix with no lesions or friability. Bimanual examination reveals a retroverted uterus. Transvaginal ultrasound shows an intrauterine pregnancy with cardiac activity; crown-rump length is consistent with gestational age. In addition to routine prenatal laboratory testing, which of the following should be offered to this patient today?
CorrectIncorrect -
Question 18 of 40
18. Question
A 22-year-old woman comes to the emergency department with fever and abdominal pain. A week ago, the patient had an elective abortion at an outside facility. For the past 3 days, she has had increasingly purulent vaginal discharge, bleeding, and intermittent headaches. The patient has no nausea, vomiting, or diarrhea. She has no chronic medical conditions or previous surgeries. Temperature is 39 C (102.2 F), blood pressure is 93/52 mm Hg, pulse is 120/min, and respirations are 18/min. The lungs are clear to auscultation bilaterally. Abdominal palpation demonstrates bilateral lower quadrant tenderness but no masses, rebound, or guarding. Purulent cervical discharge is noted on speculum examination. Bimanual pelvic examination shows an 8-week-sized, tender uterus with cervical motion tenderness; no adnexal masses are palpated. Bedside ultrasound reveals a 2 × 2 cm echogenic mass in the endometrial cavity near the uterine fundus. Urine pregnancy test is positive. Intravenous fluids and broad-spectrum antibiotics are administered. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 19 of 40
19. Question
The following vignette applies to the next 2 items.
A 22-year-old primigravida comes to the office at 13 weeks gestation for her first prenatal visit. The patient was unaware that she was pregnant until last week, when she went to the emergency department for persistent vomiting; ultrasonography confirmed an intrauterine pregnancy. The patient has irregular menstrual cycles due to polycystic ovary syndrome. Nine months ago, she stopped taking oral contraceptives due to intolerable adverse effects; she did not inform her provider. The patient also has a history of idiopathic seizures beginning in childhood and receives valproate monotherapy. She states, “I just read in one of those maternity books that seizure medications can be bad for my baby. Should I stop now? I have not had a seizure in a long time.” Her last seizure occurred a year ago after an attempt to change her medication regimen; she was hospitalized for aspiration pneumonia afterward. The patient does not use tobacco, alcohol, or recreational drugs. There is no family history of congenital abnormalities.
Item 1 of 2
Which of the following is the best strategy for management of this patient?CorrectIncorrect -
Question 20 of 40
20. Question
Item 2 of 2
This patient’s pregnancy was uneventful and she delivered a healthy baby. She has heard about the benefits of breastfeeding and asks if she can breastfeed while taking her medication. Which of the following is the most appropriate response to this patient?CorrectIncorrect -
Question 21 of 40
21. Question
A 30-year-old woman, gravida 1 para 0, at 12 weeks gestation comes to the office for an initial prenatal visit. She has had no abdominal or pelvic pain, vaginal bleeding, or leakage of fluid. The patient had mild nausea and vomiting earlier in the pregnancy that has resolved. Review of systems is negative for hematuria, dysuria, and urinary frequency. The patient has no chronic medical conditions and has had no previous surgeries. She takes a prenatal vitamin and an iron supplement daily. The patient has no known medication allergies. Blood pressure is 100/60 mm Hg and pulse is 78/min. BMI is 24 kg/m2. The fetal heart rate is 150/min by bedside Doppler ultrasound. Routine prenatal labs are collected and the results are normal except for a positive urine culture, which grows >100,000 cfu/mL pan-susceptible Streptococcus agalactiae. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 22 of 40
22. Question
A 32-year-old woman, gravida 2 para 1, at 30 weeks gestation comes to the office for a routine prenatal visit. The patient’s pregnancy has been uncomplicated, and she has had no vaginal bleeding or contractions. She has continued to jog daily throughout the pregnancy but is becoming more fatigued by the end of her workouts. The patient has no chronic medical conditions, and her only medication is a daily prenatal vitamin. She does not use tobacco, alcohol, or illicit drugs. Blood pressure is 110/70 mm Hg, pulse is 76/min, and respirations are 20/min. Fetal heart tones are normal. Physical examination is unremarkable. Compared to a nonpregnant state, this patient most likely has which of the following hematologic changes?
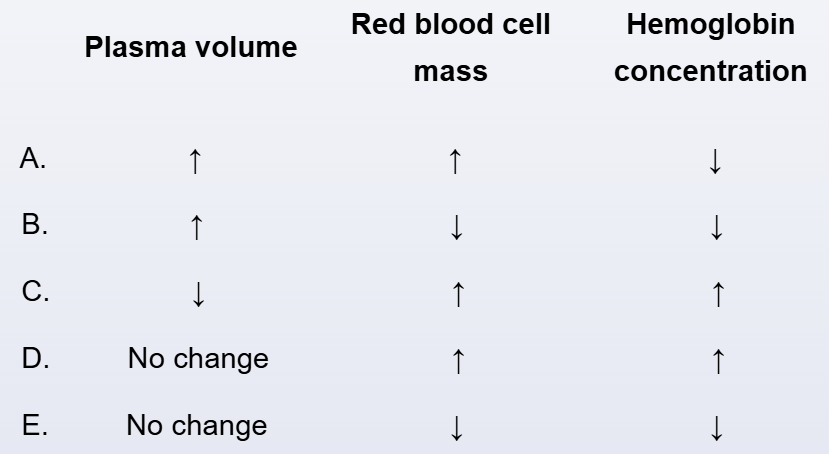 CorrectIncorrect
CorrectIncorrect -
Question 23 of 40
23. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
A 32-year-old woman, gravida 1 para 0, at 19 weeks gestation comes to the emergency department due to vaginal pressure and spotting. Over the past few days, she has had clear vaginal discharge, for which she has used sanitary napkins. Today, the patient has had increasing pelvic pressure and has noticed blood spots on the sanitary napkins. She has had no cramping or pelvic pain; fetal movement has been normal. The patient’s pregnancy was previously uncomplicated; initial prenatal laboratory testing was normal. She was scheduled to have an anatomy ultrasound later in the week. The patient has no chronic medical conditions and has had no previous surgeries. She takes a prenatal vitamin daily and acetaminophen as needed for headaches. She was treated for Chlamydia trachomatis cervicitis at age 20. The patient does not use tobacco, alcohol, or recreational drugs. Temperature is 36.7 C (98.1 F), blood pressure is 110/70 mm Hg, pulse is 65/min, and respirations are 18/min. Fetal heart rate is 145/min by Doppler ultrasound. Speculum examination shows amniotic membranes bulging at the vaginal introitus. There is no blood or pooling of fluid in the vaginal vault. Nitrazine paper does not turn blue on application of the vaginal discharge. The cervix is 3 cm dilated and 100% effaced on digital examination.
Item 1 of 2
Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 24 of 40
24. Question
Item 2 of 2
The patient is informed of the examination findings. She asks about the prognosis for this pregnancy. Which of the following is the most appropriate response to the patient at this time?
CorrectIncorrect -
Question 25 of 40
25. Question
The following vignette applies to the next 2 items.
A 37-year-old woman, gravida 3 para 2, at 13 weeks gestation comes to the office for fetal aneuploidy screening. The patient had painless vaginal spotting a few weeks ago that has since resolved. Her previous 2 pregnancies ended in uncomplicated term vaginal deliveries. The patient has no chronic medical conditions. She is the vice principal at a local elementary school, volunteers as a basketball coach, and attends a yoga class 3 times a week. The patient takes a prenatal vitamin and an iron supplement daily. Blood pressure is 110/70 mm Hg and pulse is 68/min. BMI is 26 kg/m2. Fetal heart rate is 150/min. Ultrasound reveals a 13-week fetus with a normal nuchal translucency measurement and a 1.8-cm, crescent, hypoechoic area between the gestational sac and the uterus, which is consistent with a hematoma. The patient’s blood type is B, Rh positive. Fetal aneuploidy screening results are normal.
Item 1 of 2
Which of the following is the best next step in management of this patient?CorrectIncorrect -
Question 26 of 40
26. Question
Item 2 of 2
Appropriate action was taken. Given the ultrasound findings, this patient is at increased risk for which of the following complications?CorrectIncorrect -
Question 27 of 40
27. Question
A 38-year-old woman, gravida 3 para 0, at 16 weeks gestation comes to the emergency department due to leakage of fluid and vaginal bleeding. The patient noticed increasing vaginal discharge earlier today and then noticed a large gush of fluid and vaginal bleeding an hour ago. She has had 2 spontaneous abortions at 8 weeks gestation and this pregnancy was conceived through in vitro fertilization. The patient has no chronic medical conditions and has had no surgery. Temperature is 38.3 C (100.9 F), blood pressure is 110/60 mm Hg, pulse is 112/min, and respirations are 20/min. The uterus is tender on abdominal examination. Pelvic examination confirms rupture of membranes and the cervix is 2 cm dilated. Transabdominal ultrasound shows minimal amniotic fluid and a footling breech fetus measuring 16 weeks gestation with a heart rate of 175/min. The physician explains that the patient has rupture of membranes and signs of infection. The patient starts to cry and says she wants everything done for the pregnancy if possible. Which of the following is the most appropriate management of this patient?
CorrectIncorrect -
Question 28 of 40
28. Question
A 40-year-old woman, gravida 3 para 0 aborta 2, at 16 weeks gestation comes to the office for prenatal care. She reports no abdominal pain, vaginal bleeding, or leakage of fluid. She has a history of polycystic ovary syndrome and required in vitro fertilization for all of her pregnancies. This pregnancy was complicated by first-trimester vaginal bleeding, which resolved spontaneously. A prophylactic cerclage was placed 2 weeks ago because her first 2 pregnancies ended with painless spontaneous abortions at 18 weeks gestation. The patient also has a history of type 2 diabetes mellitus and chronic hypertension, both managed with oral medications. She takes a daily prenatal vitamin with iron supplementation. She does not use tobacco, alcohol, or recreational drugs. Prior to her in vitro fertilization, the patient did hot yoga 2 days a week and jogged for 30-45 minutes approximately 3 days a week, which she would like to resume. Blood pressure is 140/90 mm Hg and pulse is 88/min. BMI is 30 kg/m2. The fetal heart rate is 150/min by Doppler sonography. Laboratory results are as follows:
Blood
Hemoglobin
10 g/dL
Platelets
240,000/mm3
Hemoglobin A1c
8.8%
Rapid plasma reagin
not detected
HIV screening
negative
Urinalysis
Protein
trace
Glucose
negative
Which of the following is the best recommendation for this patient regarding exercise during pregnancy?
CorrectIncorrect -
Question 29 of 40
29. Question
A 32-year-old woman, gravida 3 para 2, at 12 weeks gestation comes to the office to initiate prenatal care. The patient has had some fatigue and breast tenderness but no vaginal bleeding or abdominal pain. Prior pregnancies in her late 20s ended with painless spontaneous vaginal deliveries at 20 and 21 weeks gestation. The patient has no chronic medical conditions and takes no daily medications. At age 24, she underwent a cold knife cone procedure for high-grade cervical intraepithelial neoplasia. All subsequent Pap and human papillomavirus testing has been negative. Blood pressure is 110/60 mm Hg. BMI is 24 kg/m2. Pelvic examination reveals a 12-week-sized uterus with a closed cervix and no adnexal masses or tenderness. Speculum examination shows a nonfriable cervix with no visible lesions. Transvaginal ultrasound reveals a 12-week intrauterine gestation with a normal fetal heart rate. The patient asks about preventing another preterm delivery. Which of the following is the best management option for this patient?
CorrectIncorrect -
Question 30 of 40
30. Question
A 32-year-old woman, gravida 1 para 0, at 38 weeks comes to labor and delivery with contractions and rupture of membranes. She has had no vaginal bleeding and fetal movement is normal. The patient has received consistent prenatal care, and her pregnancy has been complicated by insulin-controlled gestational diabetes mellitus. She has no chronic medical conditions or previous surgeries. Temperature is 36.7 C (98.1 F), blood pressure is 152/98 mm Hg, pulse is 112/min, and respirations are 24/min. Fetal heart rate shows a baseline of 150/min with accelerations and multiple variable decelerations. Tocodynamometer shows contractions every 3 minutes. Cervical examination reveals that the cervix is 7 cm dilated with a fetal chin palpated posteriorly at −2 station and the fetal brow behind the maternal pubic symphysis. Fingerstick glucose is 120 mg/dL. Urinalysis has 1+ glucose and is negative for protein. An urgent cesarean delivery is recommended. Which of the following is the indication for cesarean delivery in this patient?
CorrectIncorrect -
Question 31 of 40
31. Question
The following vignette applies to the next 2 items.
A 42-year-old woman, gravida 6 para 6, is evaluated in the postpartum unit on postoperative day 2 after a cesarean delivery. The patient has had increasing vaginal bleeding, abdominal pain, and fever. She is breastfeeding exclusively with a good latch. The patient was initially admitted to the hospital for prelabor rupture of membranes at 40 weeks gestation. The patient had a negative Group B Streptococcus rectovaginal culture. A primary cesarean delivery was performed for arrest of descent of a 5-kg (11-lb) infant after 3 hours of pushing. The pregnancy was complicated by recurrent vaginal candidiasis. Prior pregnancies were uncomplicated; the patient’s last delivery was 12 years ago. Temperature is 38.7 C (101.7 F), blood pressure is 110/70 mm Hg, pulse is 114/min, and respirations are 18/min. On physical examination, the patient appears pale and tired. The lungs are clear to auscultation bilaterally; the breasts are full but without erythema. The uterine fundus is tender to palpation. Speculum examination shows heavy lochia but no active bleeding. The transverse incision across the lower abdomen is intact and without erythema or drainage.
Item 1 of 2
Which of the following is the most appropriate pharmacotherapy for this patient?CorrectIncorrect -
Question 32 of 40
32. Question
Item 2 of 2
Which of the following is this patient’s most important risk factor for her current postpartum infection?CorrectIncorrect -
Question 33 of 40
33. Question
A 25-year-old woman, gravida 1 para 0 aborta 1, comes to the office for a preconception counseling visit. Her sister recently developed abruptio placentae after a motor vehicle accident and underwent an emergency cesarean delivery at 32 weeks gestation. The patient had been considering stopping her oral contraceptive pills to conceive but is now feeling apprehensive about pregnancy complications after what happened to her sister. She has a history of generalized anxiety disorder and major depression. Her only surgery was a suction curettage for an elective abortion 5 years ago. In addition to oral contraceptive pills, the patient takes a selective serotonin reuptake inhibitor and multivitamin daily. Family history is noncontributory. The patient does not use alcohol, tobacco, or illicit drugs. She reports feeling safe at home. All her vaccinations are up to date. She works as a babysitter for elementary school children, with the responsibilities of driving them to after-school activities and preparing meals. The patient enjoys running and competes in 1 or 2 marathons a year. BMI is 23 kg/m2. Physical examination is within normal limits. She is considering quitting her job when she becomes pregnant and asks what else she can do to decrease her risk of complications in pregnancy. Which of the following is the best response?
CorrectIncorrect -
Question 34 of 40
34. Question
A 33-year-old woman, gravida 2 para 1, at 33 weeks gestation comes to the emergency department due to continuous leakage of fluid that began 2 hours ago. The fluid is clear and not malodorous, and she has had no contractions or vaginal bleeding. Fetal movement is normal. This pregnancy was complicated by bacterial vaginosis in the first trimester that resolved after a course of antibiotics. Her previous pregnancy ended in a vaginal delivery at 37 weeks gestation after induction of labor for prelabor rupture of membranes. The patient has no chronic medical conditions and has had no previous surgeries. Temperature is 36.7 C (98.1 F), blood pressure is 110/68 mm Hg, and pulse is 92/min. The uterine fundus is nontender. On speculum examination, there is a clear pool of fluid that is nitrazine positive and crystallizes in a fern-like pattern after drying on a slide. The cervix appears visibly closed; digital cervical examination is deferred. The fetal heart rate tracing demonstrates a normal baseline, moderate variability, accelerations, and no decelerations. Transabdominal ultrasound reveals a fetus in vertex presentation and an amniotic fluid index of 3 cm. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 35 of 40
35. Question
A 41-year-old woman comes to the emergency department due to worsening shortness of breath. The patient had an uncomplicated vaginal delivery 8 days ago. She initially experienced dyspnea only when walking, but now she “cannot catch her breath” even at rest. The patient has been breastfeeding her infant every 2-3 hours and says that this schedule is making her anxious and fatigued throughout the day. She tries to sleep when her infant does but has increasing symptoms when lying down. The patient has had no fevers, chills, chest pain, or abdominal pain. She has ongoing vaginal bleeding that partially saturates a menstrual pad every 3-4 hours. The patient has no chronic medical conditions and has had no previous surgeries. Temperature is 37 C (98.6 F), blood pressure is 172/105 mm Hg, pulse is 70/min, and respirations are 24/min. Pulse oximetry is 92% on room air. Cardiac examination shows a regular rhythm. The neck veins are flat. Auscultation of the lungs demonstrates diffuse bilateral rales. There is 3+ pitting edema to the knees. Deep tendon reflexes are 4+ bilaterally with multiple beats of clonus. Which of the following is the most likely diagnosis in this patient?
CorrectIncorrect -
Question 36 of 40
36. Question
The following vignette applies to the next 3 items.
A 27-year-old woman, gravida 1 para 0, at 28 weeks gestation comes to the office for a routine prenatal visit. Her initial prenatal laboratory results at 12 weeks gestation were as follows:
Hemoglobin
11.8 g/dL
Mean corpuscular volume
84 µm3
Platelets
180,000/mm3
Leukocytes
7,500/mm3
Urine culture
Negative
The patient reports no vaginal bleeding, leakage of fluid, or contractions. There is good fetal movement. She has increasing urinary frequency and nocturia but no dysuria or hematuria. The patient has a history of tension headaches, which have become more frequent but resolve with acetaminophen. She has no other chronic medical conditions or previous surgeries. The patient works in a retirement home and reports leg swelling at the end of her shift. She is a vegetarian and takes a daily prenatal vitamin. She does not use tobacco, alcohol, or illicit drugs. Temperature is 37 C (98.6 F), blood pressure is 128/76 mm Hg, and pulse is 86/min. BMI is 30 kg/m2; the patient has been gaining 0.5 kg (1.1 lb) a week during the pregnancy. The fetal heart rate is 152/min. Examination shows a uterus consistent with a 28-week gestation. There is trace lower extremity edema bilaterally. The patient has had no laboratory evaluations since her initial prenatal visit.
Item 1 of 3
Which of the following is the most appropriate laboratory evaluation to perform at this visit?
CorrectIncorrect -
Question 37 of 40
37. Question
Item 2 of 3
The patient’s test results from the 28-week prenatal visit are as follows:
Hemoglobin
10.6 g/dL
Hematocrit
33%
Mean corpuscular volume
86 fL
Platelets
90,000/mm3
Leukocytes
9,000/mm3
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 38 of 40
38. Question
Item 3 of 3
The patient comes to the hospital at 38 weeks gestation in active labor and with spontaneous rupture of membranes. Blood pressure is 130/84 mm Hg and heart rate is 96/min. Fetal heart rate tracing is reassuring. Uterine contractions are regular and occur every 4 minutes. Cervical examination reveals 5-cm dilation, 100% effacement, and a vertex presentation at −1 station. Complete blood count on admission is as follows:
Hemoglobin
9.6 g/dL
Hematocrit
28%
Platelets
102,000/mm3
The patient requests neuraxial labor analgesia.
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 39 of 40
39. Question
A 19-year-old woman, gravida 1 para 0, comes to the office at 28 weeks gestation for a routine prenatal visit. Her prenatal course was complicated by vaginal bleeding at 8 weeks gestation due to a subchorionic hematoma. At that time, laboratory evaluation in the emergency department showed that she was Rh(D) negative, and she received anti-D immune globulin. The vaginal bleeding resolved, and the patient has had no other problems during this pregnancy. She has no chronic medical problems or previous surgeries. The patient does not use tobacco, alcohol, or illicit drugs. Blood pressure is 110/70 mm Hg and heart rate is 80/min. Fundal height is 28 cm and fetal heart rate is 145/min. Laboratory evaluation today shows a negative anti-D antibody screen. The patient is no longer in contact with the father of her child, and his Rh(D) status is unknown. Which of the following is the best next step concerning Rh(D) alloimmunization in this patient?
CorrectIncorrect -
Question 40 of 40
40. Question
A 25-year-old woman, gravida 1 para 0, at 8 weeks gestation comes to the emergency department due to nausea and vomiting. The patient has had nausea and vomiting once or twice a day for the past 2 weeks; today, she has vomited 3 times, but has been able to tolerate liquids and small snacks. She has no fever, chills, diarrhea, or sick contacts. The patient has had no vaginal bleeding, dysuria, or abdominal pain. She has gastroesophageal reflux disease, and has been following a diet of small, frequent, bland meals. The patient takes a daily prenatal vitamin and H2 receptor antagonist. Temperature is 36.7 C (98.1 F), blood pressure is 100/60 mm Hg, and heart rate is 80/min. Weight is 50 kg (110.2 lb), a 0.8-kg (1.8-lb) increase from her prepregnancy weight. Mucous membranes are moist. Cardiac examination shows a regular rate and rhythm with no murmurs. The abdomen is soft, nontender, and nondistended. Serum electrolytes are normal. Urine dipstick is negative for ketones. Transvaginal ultrasound reveals an intrauterine pregnancy with cardiac activity at 160/min, and a crown-rump length consistent with an 8-week gestation. Which of the following is the most appropriate management for this patient?
CorrectIncorrect
