Time limit: 0
Quiz Summary
0 of 24 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Quiz complete. Results are being recorded.
Results
0 of 24 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 24
1. Question
A 32-year-old woman, gravida 1 para 0, calls the office to schedule her first prenatal visit. Her last menstrual period was 5 weeks ago and she had a positive pregnancy test 2 days ago. The patient feels well and has no vaginal bleeding or cramping. She was diagnosed with Hashimoto thyroiditis 4 years ago and has been on a stable dose of levothyroxine for the past 2 years. Serum TSH 3 months ago was within normal limits. The patient has no other chronic medical conditions or previous surgeries. She has started taking a prenatal vitamin daily. Family history is significant for a sister currently undergoing evaluation for recurrent miscarriages. The patient does not use tobacco, alcohol, or illicit drugs. She is nervous about her sister’s obstetric history and asks if she needs to make any changes to her medication. Which of the following would be the most appropriate response to this patient?
CorrectIncorrect -
Question 2 of 24
2. Question
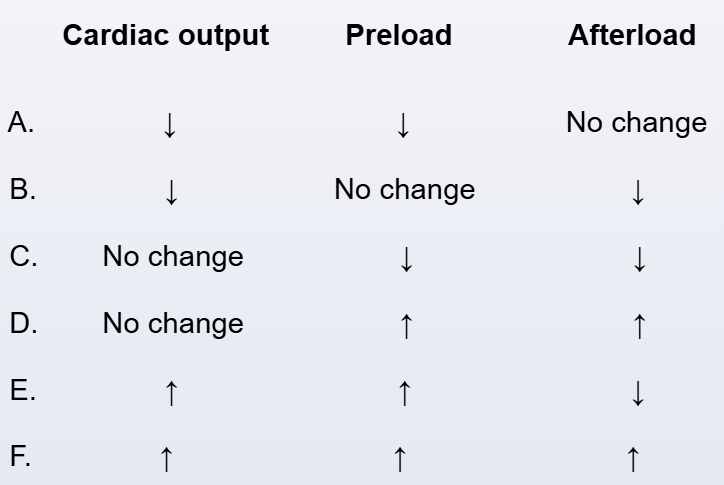
A 36-year-old woman, gravida 2 para 1, at 30 weeks gestation comes to the office for a prenatal visit. The patient has noticed some ankle swelling at the end of the day that is relieved with elevating her legs, but she has no other concerns. The pregnancy has been uncomplicated, and her only medications are a prenatal vitamin and iron supplement. The patient has no chronic medical conditions. She does not use tobacco or alcohol. Blood pressure is 118/78 mm Hg and pulse is 72/min. BMI is 30 kg/m2. Fetal heart tones are normal. There is trace bilateral pedal edema to the shins. Physical examination is otherwise unremarkable. Urinalysis shows no protein. Compared to a nonpregnant state, which of the following cardiac changes are most likely to be found in this patient?
 CorrectIncorrect
CorrectIncorrect -
Question 3 of 24
3. Question
A 32-year-old pregnant woman at 18 weeks gestation comes to the emergency department due to severe right-sided abdominal pain for 6 hours. The patient rates the pain as 10 on a scale of 0-10. The pain is crampy and paroxysmal and radiates to the labia. When the pain occurs, she has associated nausea and vomiting. The patient has no vaginal bleeding, fever, hematuria, or dysuria. She underwent cesarean delivery with her first child 3 years ago. The pregnancy thus far had been uncomplicated, and initial prenatal laboratory testing was normal. On examination, the patient is unable to find a comfortable position. Temperature is 36.7 C (98.1 F), blood pressure is 110/60 mm Hg, and pulse is 106/min. BMI is 32 kg/m2. The abdomen is soft, nontender, and nondistended to palpation. There is no costovertebral angle or suprapubic tenderness. Pelvic examination shows an 18-week-sized uterus. Laboratory results are as follows:
Complete blood count
Hemoglobin
11.2 g/dL
Platelets
180,000/mm3
Leukocytes
13,000/mm3
Which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 4 of 24
4. Question
A 23-year-old primigravida comes to the clinic at 9 weeks gestation for prenatal counseling. She reports a family history of hemophilia A and expresses concern about her child having hemophilia. The patient and her husband have no history of abnormal bleeding. A pedigree of the woman’s family is shown below; she is represented by II-8.
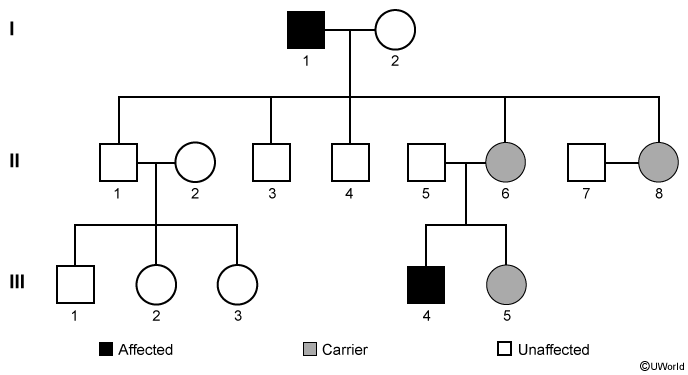
Which of the following best states the patient’s risk related to hemophilia?
CorrectIncorrect -
Question 5 of 24
5. Question
The following vignette applies to the next 2 items.
A 38-year-old woman, gravida 3 para 3, comes to the office due to a 2-week history of dysuria and pain on deep penetration during sexual intercourse. For the past few months, urine dribbling has occurred after she voids. The patient has no fever, chills, hematuria, nocturia, or increased urinary frequency. Medical history is notable for multiple urinary tract infections. She has regular, monthly menses with 4 days of moderate bleeding. The patient’s last pregnancy was 4 years ago, and all resulted in uncomplicated term vaginal deliveries. Temperature is 36.7 C (98.1 F), blood pressure is 120/80 mm Hg, and pulse is 78/min. The abdomen is soft and nontender, with no palpable masses. There is no costovertebral angle tenderness. Pelvic examination shows a tender area of fullness along the anterior vaginal wall. The uterus is small, mobile, and nontender; there are no adnexal masses. Laboratory results are as follows:
Urinalysis
Color
yellow
Turbidity
cloudy
pH
6.2
Specific gravity
1.015
Protein
negative
Glucose
negative
Ketones
negative
Blood
positive
Leukocyte esterase
positive
Nitrite
positive
White blood cells
20-30/hpf
Red blood cells
4/hpf
Item 1 of 2
Which of the following is the most likely diagnosis for this patient?CorrectIncorrect -
Question 6 of 24
6. Question
Item 2 of 2
Which of the following is the best next step in diagnosing this patient’s condition?CorrectIncorrect -
Question 7 of 24
7. Question
The following vignette applies to the next 2 items.
A 29-year-old woman, gravida 1 para 0, at 26 weeks gestation comes to the office for a routine prenatal visit. She has had no contractions, vaginal bleeding, or leakage of fluid. There is good fetal movement. The patient has a history of polycystic ovary syndrome. This pregnancy was conceived through ovulation induction but has otherwise been uncomplicated. Results of prenatal laboratory testing from her initial visit at 8 weeks gestation include a hemoglobin A1c of 5.6%. She has no other chronic medical conditions or previous surgeries. The patient walks for 30-45 minutes 5 days a week. She takes prenatal vitamins and a folate supplement daily. Blood pressure is 130/80 mm Hg and pulse is 89/min. BMI is 27 kg/m2. Fetal heart tones are 150/min. Fundal height is 28 cm. Laboratory results from today’s visit are as follows:
Hemoglobin
11.2 g/dL
Platelets
160,000/mm3
1-hour 50-g glucose challenge test
145 mg/dL (normal: <140)
Rapid plasma reagin
nonreactive
Item 1 of 2
Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 8 of 24
8. Question
Item 2 of 2
Appropriate evaluation of the patient is completed, and gestational diabetes mellitus is diagnosed. She is instructed to start a diabetic diet and continue to exercise regularly, with an hour of brisk walking on most days. The patient returns 2 weeks later for a routine prenatal visit and for evaluation of her glycemic control. She reports compliance with diet and exercise and has been checking her fasting and postprandial blood glucose values daily. Blood pressure is 136/70 mm Hg and pulse is 80/min. Fetal heart tones are 140/min. During the third week of the patient’s regimen, fasting blood glucose values are 110-130 mg/dL (normal: ≤95), and 2-hour postprandial glucose values are 138-168 mg/dL (normal: ≤120). The physician recommends insulin initiation. The patient states, “I really don’t like needles and don’t think I can give myself injections.” Which of the following is the best response to this patient?
CorrectIncorrect -
Question 9 of 24
9. Question
A 22-year-old woman comes to the office to discuss initiating oral contraception. She has been sexually active with the same partner for the last year and has been using condoms but would like a more reliable method of contraception. The patient has a 4-year history of primary hypothyroidism, which has been well controlled on 125 µg/day of levothyroxine. Her most recent serum TSH was within normal limits. She has no other chronic medical conditions and no previous surgeries. The patient does not use tobacco, alcohol, or illicit drugs. Family history is significant for breast cancer in her mother diagnosed at age 52 and a sister who has type 1 diabetes mellitus. Blood pressure is 110/76 mm Hg and pulse is 78/min. BMI is 24 kg/m2. There is no thyromegaly, and the remainder of the physical examination is normal. The patient states that her best friend noted an improvement in her acne after starting an oral contraceptive, and she would like to take the same type of pill. Which of the following is the most accurate statement regarding contraception in this patient?
CorrectIncorrect -
Question 10 of 24
10. Question
A 28-year-old woman comes to the office after finding a lump in her right breast. Her mother died from ovarian cancer at age 34 and her maternal aunt died from breast cancer at age 32. After an appropriate workup, the patient is diagnosed with breast cancer. This patient most likely inherited a mutation in a gene normally responsible for which of the following processes?
CorrectIncorrect -
Question 11 of 24
11. Question
A 32-year-old woman, gravida 3 para 2, comes to the office at 10 weeks gestation to establish prenatal care. She has mild nausea and anxiety and has not gained weight because of decreased food intake due to the nausea. The patient’s first pregnancy was complicated by hyperemesis gravidarum, but her second was uneventful. She has no chronic medical conditions, and her only medication is a daily prenatal vitamin. Blood pressure is 122/82 mm Hg and pulse is 94/min and regular. The thyroid gland is normal to palpation. There is no lid-lag or proptosis. Laboratory results show a serum TSH of 0.3 µU/mL. Which of the following is the best next step in management of this patient’s thyroid function?
CorrectIncorrect -
Question 12 of 24
12. Question
The following vignette applies to the next 2 items. The items in the set must be answered in sequential order. Once you click Proceed to Next Item, you will not be able to add or change an answer.
An 18-year-old woman comes to the office due to painful urination and urinary frequency. The patient is sexually active with her boyfriend and has had painful intercourse the past 3 days. She has no fever, chills, nausea, vomiting, or flank pain. The patient uses condoms consistently for contraception, and her last menstrual period was 4 weeks ago. She has no chronic medical conditions or surgeries and has no known drug allergies. Temperature is 37.8 C (100 F), blood pressure is 110/70 mm Hg, pulse is 82/min, and respirations are 18/min. Mild suprapubic tenderness is present on abdominal examination. Pelvic examination shows clear, thin vaginal discharge with no cervical motion tenderness. The remainder of the examination is normal. Urinalysis shows positive leukocyte esterase, positive nitrites, and 10 red blood cells/hpf. The physician considers prescribing a 1-week course of trimethoprim-sulfamethoxazole.
Item 1 of 2
Prior to initiating treatment, which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 13 of 24
13. Question
Item 2 of 2
The pregnancy test result is positive. Which of the following is the most appropriate treatment for this patient’s presenting symptoms?
CorrectIncorrect -
Question 14 of 24
14. Question
A 30-year-old woman comes to the office for preconception counseling. She has a history of rheumatic heart disease and underwent mechanical mitral valve replacement 5 years ago. The patient has been taking warfarin and low-dose aspirin since the procedure and has had no complications or adverse reactions. She has no history of other chronic medical conditions or surgeries. The patient recently began taking folic acid daily and is planning on discontinuing her progestin-releasing intrauterine device in the next few months. She does not use tobacco, alcohol, or illicit drugs. Family history is significant for a grandmother with a recent hip replacement complicated by a postoperative pulmonary embolism. Blood pressure is 110/70 mm Hg and pulse is 78/min. BMI is 23 kg/m2. Physical examination is without abnormalities, other than a large sternotomy scar. The patient expresses concern about the possible adverse effects of warfarin on the baby and her pregnancy. Which of the following is the most appropriate recommendation for this patient?
CorrectIncorrect -
Question 15 of 24
15. Question
A 24-year-old woman, gravida 1 para 0, at 12 weeks gestation comes to the office for an initial prenatal visit. She is doing well and has no vaginal bleeding or cramping. The patient has a history of cystitis that occurred prior to pregnancy but currently has no dysuria or hematuria. She has no chronic medical conditions or previous surgeries. The patient takes a prenatal vitamin daily and has no known medication allergies. She does not use tobacco, alcohol, or recreational drugs. Temperature is 36.7 C (98 F), blood pressure is 124/74 mm Hg, and pulse is 78/min. Fetal heart rate is 140/min by Doppler ultrasonography. Physical examination is otherwise unremarkable. A routine clean catch urine culture from today’s visit grows >100,000 colony-forming units/mL of Escherichia coli. Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 16 of 24
16. Question
A 28-year-old woman, gravida 2 para 0 aborta 2, comes to the office for follow-up after a suction curettage 2 weeks ago for an empty gestational sac. The patient has had light vaginal spotting since the procedure, but no heavy vaginal bleeding or passage of clots. She has had no fever, abdominal pain, or abnormal vaginal discharge. The patient has no chronic medical conditions and has had no previous surgeries. A year ago, she had a left-sided ectopic pregnancy that was treated with methotrexate. She has no history of sexually transmitted infections. Family history is noncontributory. The patient does not use tobacco, alcohol, or illicit drugs. She has no drug allergies. Temperature is 36.7 C (98 F) and blood pressure is 120/60 mm Hg. BMI is 24 kg/m2. Pelvic examination shows a nontender, 6-week-sized uterus and no adnexal masses or tenderness. Speculum examination reveals scant dark blood in the vaginal vault but no active bleeding or abnormal discharge. The pathology report indicates hyperplastic and hydropic trophoblastic villi but no fetal tissue, consistent with a hydatidiform mole. In addition to starting contraception, which of the following is the most appropriate next step in management of this patient?
CorrectIncorrect -
Question 17 of 24
17. Question
A 32-year-old woman, gravida 1 para 1, comes to the office for preconceptual counseling. A year ago, the patient’s pregnancy was complicated by congestive heart failure diagnosed at 36 weeks gestation when she developed fatigue and shortness of breath. Evaluation at that time revealed a left ventricular ejection fraction of 20%. The patient subsequently underwent a preterm induction of labor and had a vaginal delivery. She was started on carvedilol and lisinopril, which she continues to take without side effects. A follow-up echocardiogram at 6 months postpartum showed an improving ejection fraction. The patient tolerates daily activities and has no chest pain, shortness of breath, syncope, or lower extremity swelling. She has no other chronic medical conditions and has had no surgeries. The patient does not use tobacco, alcohol, or illicit drugs. She is considering another pregnancy and would like an assessment of her risk. Which of the following provides the best prognostic information regarding this patient’s risk during a future pregnancy?
CorrectIncorrect -
Question 18 of 24
18. Question
A 22-year-old woman comes to the physician at 8 weeks gestation for routine prenatal counseling. Her husband has hemophilia A. Her own family history is insignificant. She is concerned about the possibility of her child having hemophilia. Which of the following is the best response to her questions?
CorrectIncorrect -
Question 19 of 24
19. Question
A 35-year-old woman, gravida 2 para 1, at 20 weeks gestation comes to the office due to cholelithiasis found incidentally during a prenatal ultrasound. She has no prior history of gallstones and has no abdominal pain, jaundice, or clay-colored stool. She has no chronic medical conditions, and her only medication is a daily prenatal vitamin. The patient stopped drinking alcohol after learning that she was pregnant and does not use tobacco or recreational drugs. Her mother underwent cholecystectomy for acute cholecystitis at age 40. Vital signs are within normal limits. The patient is anicteric, and mucous membranes are moist and pink. Examination reveals a gravid abdomen but no tenderness. Laboratory results are as follows:
Complete blood count
Hemoglobin
10.8 mg/dL
Platelets
240,000/mm3
Leukocytes
7,500/mm3
Liver function studies
Total bilirubin
0.8 mg/dL
Alkaline phosphatase
50 U/L
Aspartate aminotransferase
18 U/L
Alanine aminotransferase
24 U/L
Lipase
30 U/L
Ultrasonography of the right upper quadrant reveals a 1-cm gallstone without gallbladder distension, wall thickening, or pericholecystic fluid. The intrahepatic biliary ducts and common bile duct are normal in size. Which of the following is the most appropriate intervention for this patient’s gallstone?
CorrectIncorrect -
Question 20 of 24
20. Question
A 52-year-old woman comes to the office for an annual examination. The patient reports increased urinary frequency and involuntary leakage of urine for the past several years. The leakage occurs when she stands up, sneezes, or coughs. The patient manages the leakage by wearing a pad, but for the past 6 months she has needed to use 2 or 3 pads daily. She reports no dysuria or hematuria. The patient has type 2 diabetes mellitus that she manages with diet and oral medication. She has had 3 uncomplicated pregnancies, each resulting in spontaneous vaginal deliveries. The patient has smoked a quarter of a pack of cigarettes daily for the last 30 years and drinks alcohol socially, but she does not use illicit drugs. She drinks 2 cups of coffee each morning and a glass of caffeinated diet soda with dinner. Blood pressure is 130/84 mm Hg and pulse is 76/min. BMI is 29 kg/m2. A pelvic examination shows a small anteverted, nontender uterus and no adnexal masses. The vagina is pale and without rugae. During examination, leakage of urine occurs with coughing while lying down and standing. Results of urinalysis are normal. Which of the following additional tests is required prior to recommending treatment for this patient’s condition?
CorrectIncorrect -
Question 21 of 24
21. Question
A 26-year-old woman, gravida 1 para 0, comes to the office to initiate prenatal care. The patient has had no nausea, abdominal pain, or vaginal bleeding since her last menstrual period 8 weeks ago. She has no chronic medical conditions. She had an appendectomy as a child but no other surgery. The patient takes a daily prenatal vitamin and does not use tobacco, alcohol, or illicit drugs. She is a vegetarian and emigrated from Southeast Asia 5 years ago. Blood pressure is 110/75 mm Hg and pulse is 80/min. BMI is 21 kg/m2. Pelvic examination reveals an 8-week-sized, nontender uterus and no adnexal masses or tenderness. Laboratory results are as follows:
Hemoglobin
10.4 g/dL
Platelets
210,000/mm3
Leukocytes
5,200/mm3
Mean corpuscular volume
68 fm3 (normal: 80-96 fm3)
Mean corpuscular hemoglobin
22 pg/cell (normal: 28-32 pg/cell)
Red blood cells
5.6 million/mm3 (normal: 3.6-5.0 million/mm3)
Red cell distribution width
14.2% (normal: 11.5%-14.5%)
Ferritin
316 ng/mL (normal: 15-200 ng/mL)
A transvaginal ultrasound reveals an 8-week intrauterine gestation with a normal heartbeat. Which of the following is the most likely cause of this patient’s anemia?
CorrectIncorrect -
Question 22 of 24
22. Question
A 32-year-old woman is brought to the emergency department after she was found confused on the street. The patient is experiencing homelessness and lives in a shelter. She has not received medical care in several years and has no known chronic medical conditions. She has a history of intravenous drug use and smokes cigarettes. Temperature is 37.2 C (99 F), blood pressure is 120/60 mm Hg, and pulse is 94/min. BMI is 19 kg/m2. On examination, the patient is disoriented and mildly agitated. The sclerae are icteric. The mucous membranes are moist; there is poor oral hygiene and multiple dental caries. Scattered petechial lesions are present on her extremities and trunk. Heart and lung sounds are normal. Abdominal examination reveals no tenderness, but the uterus is enlarged, corresponding to a 16-week gestation. There is no focal weakness or sensory loss. Laboratory results are as follows:
Complete blood count
Hemoglobin
7.9 g/dL
Mean corpuscular volume
84 µm3
Platelets
22,000/mm3
Leukocytes
8,500/mm3
Serum chemistry
Sodium
139 mEq/L
Potassium
4.7 mEq/L
Chloride
102 mEq/L
Bicarbonate
25 mEq/L
Blood urea nitrogen
12 mg/dL
Creatinine
1.5 mg/dL
Calcium
10.1 mg/dL
Liver function studies
Total bilirubin
3.8 mg/dL
Direct bilirubin
0.8 mg/dL
Aspartate aminotransferase (SGOT)
33 U/L
Alanine aminotransferase (SGPT)
28 U/L
Urine pregnancy test is positive. Which of the following is the most likely cause of this patient’s current condition?
CorrectIncorrect -
Question 23 of 24
23. Question
A 34-year-old woman, gravida 2 para 1, at 32 weeks gestation comes to the office for routine prenatal care. The patient reports no contractions, vaginal bleeding, or leakage of fluid. Fetal movement is normal. The patient reports a dark rash on her face that she first noticed 2 weeks ago. She has applied an over-the-counter moisturizer to the rash daily for the last week but has not noticed any improvement. The patient has no chronic medical conditions and no previous surgeries. She takes a daily prenatal vitamin and does not use tobacco, alcohol, or illicit drugs. The patient has no known drug allergies. She works as an accountant and enjoys gardening on the weekends. Blood pressure is 120/80 mm Hg and pulse is 65/min. The fetal heart rate is 140/min by Doppler ultrasound. Fundal height is 32 cm. Skin examination is shown in the image below. The remainder of the physical examination is unremarkable.

Which of the following is the best next step in management of this patient?
CorrectIncorrect -
Question 24 of 24
24. Question
A 27-year-old woman, gravida 3 para 1 aborta 1, at 20 weeks gestation comes to the office as she is concerned that she might be at risk for hemolytic disease. She just learned that her sister-in-law’s second baby has hydrops fetalis due to Rh(D) incompatibility and is concerned that this could happen to her second baby as well. The patient’s pregnancy has been uncomplicated to date. The patient is Rh(D) positive and her husband is Rh(D) negative. Their 3-year-old son is healthy, and he is Rh(D) positive. A year prior, the patient had a missed abortion requiring suction curettage. She has no chronic medical problems and no other surgeries. The patient is taking a prenatal vitamin and does not use tobacco, alcohol, or illicit drugs. Vital signs are normal. Fetal anatomic ultrasound a week prior demonstrated an echogenic intracardiac focus but no other abnormalities. Which of the following is the most accurate statement to the patient regarding hemolytic disease due to Rh(D) incompatibility?
CorrectIncorrect
